
|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |

|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |
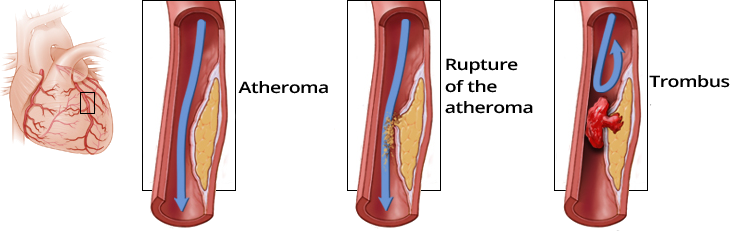
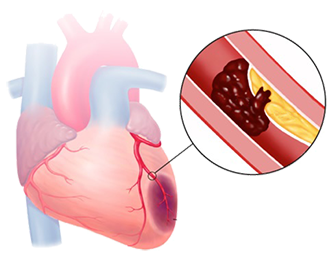
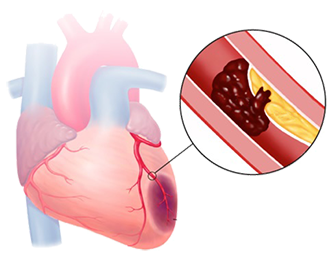
Atherosclerosis and Acute Coronary Syndrome
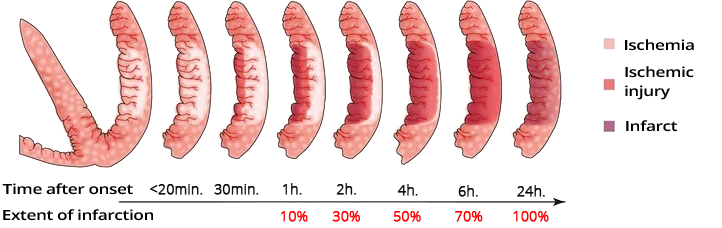
Dynamics of Ischemia after Occlusion
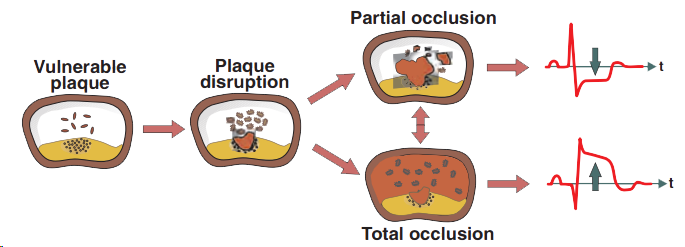
ST Segment and Acute Coronary Syndrome
Subendocardial Ischemia

Subepicardial Ischemia
Acute Coronary Syndrome
STEMI Infarction

NSTEMI Infarction
Ischemia Post-Ergometry
Unstable Angina Pectoris
Acute STEMI of the Anterior Wall
Sources
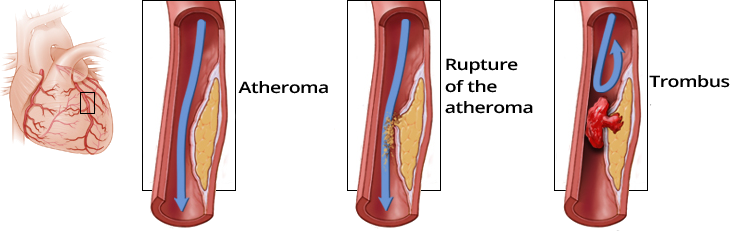
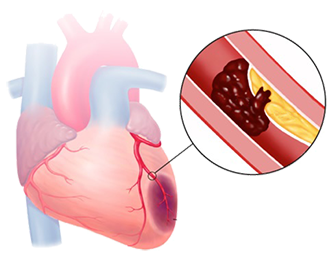
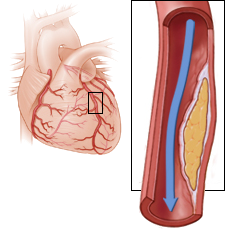
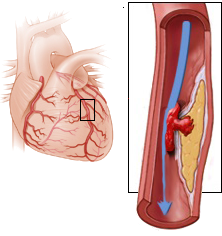
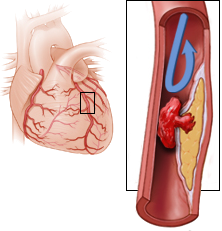
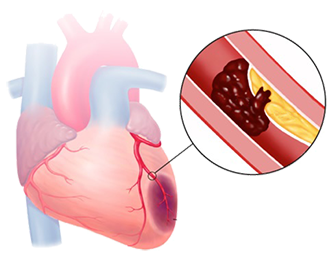
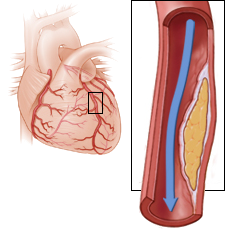
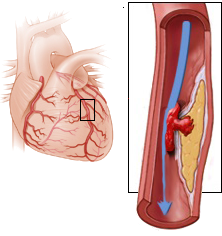
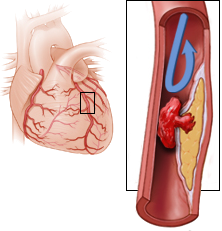
Atherosclerosis and Acute Coronary Syndrome
Dynamics of Ischemia in Occlusion
|
|
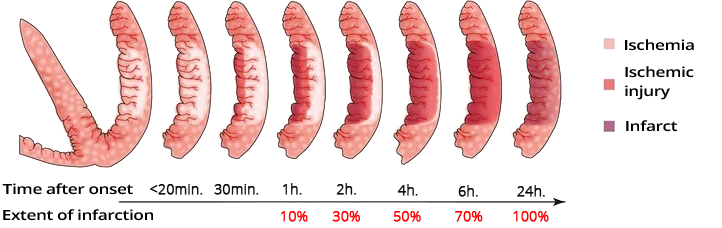
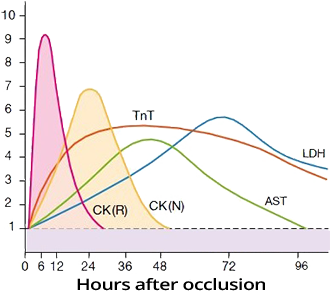
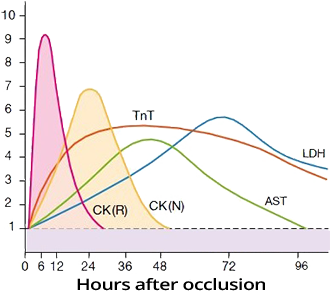
Dynamics of Ischemia after Occlusion
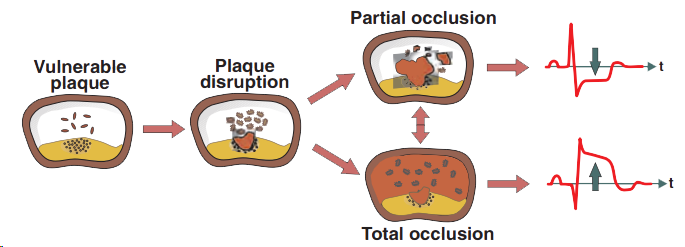
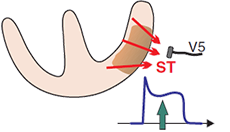
ST Segment and Acute Coronary Syndrome
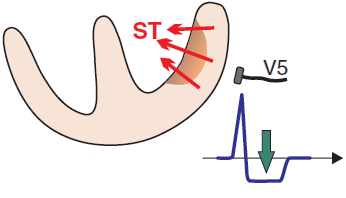
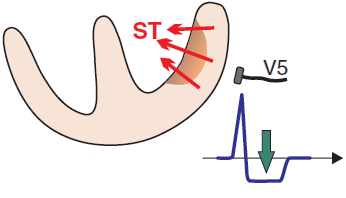
Subendocardial Ischemia
|

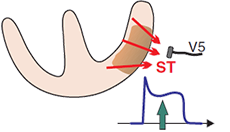
Subepicardial Ischemia
|
Troponin and Infarction
|
|
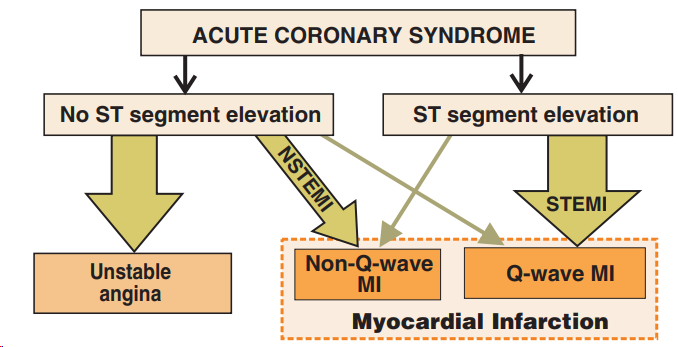
Acute Coronary Syndrome (ACS)
|
|
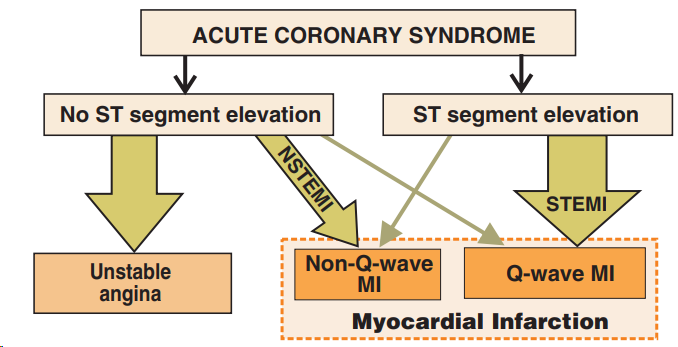
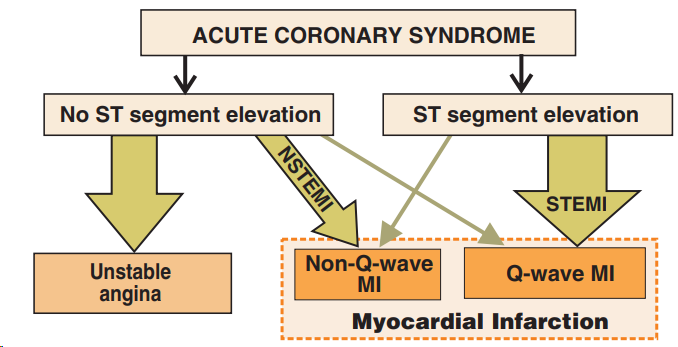
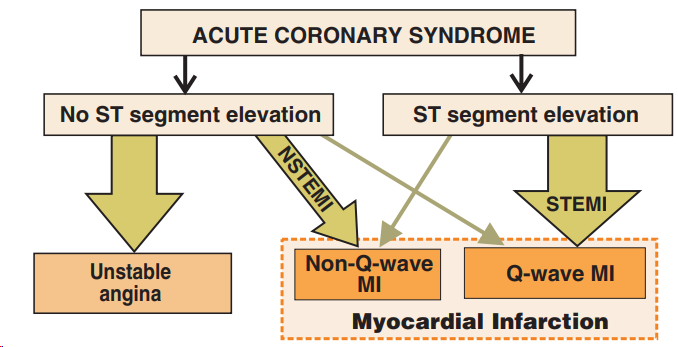
Acute Coronary Syndrome
Nomenclature of Infarction
|
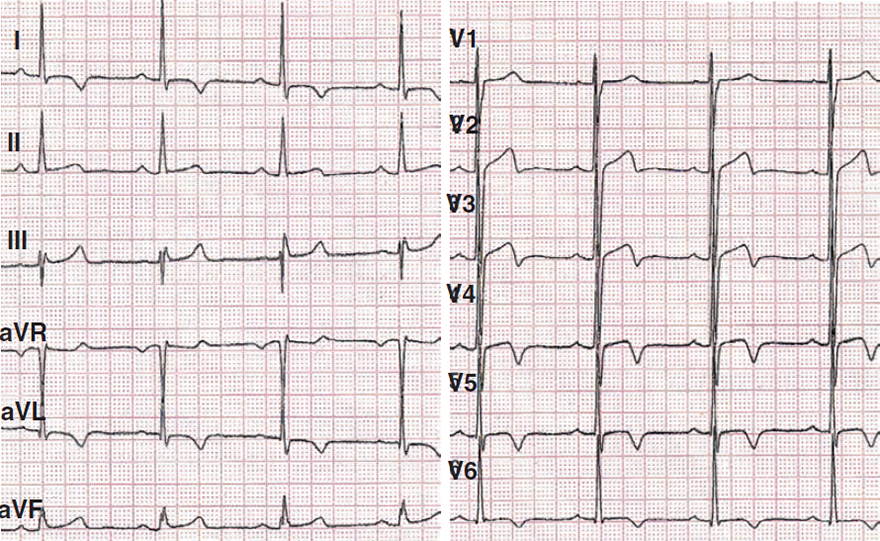
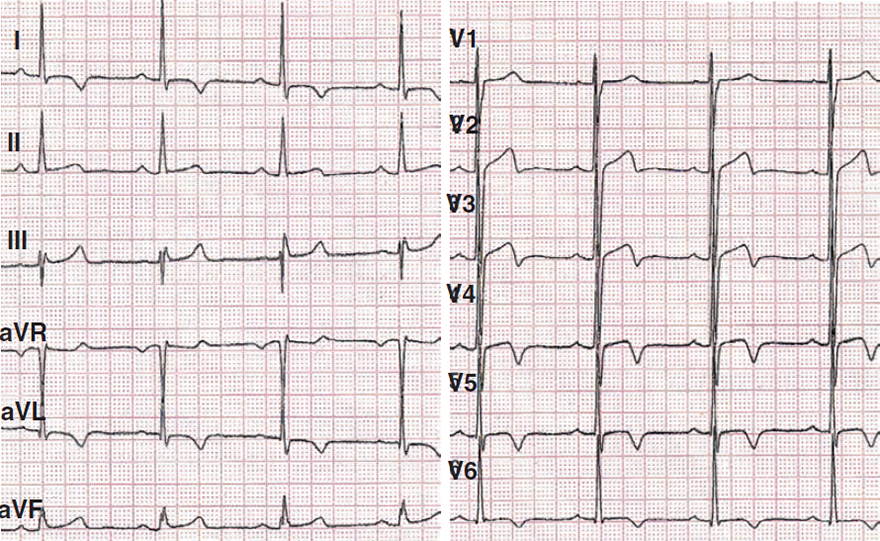
STEMI Infarction
|

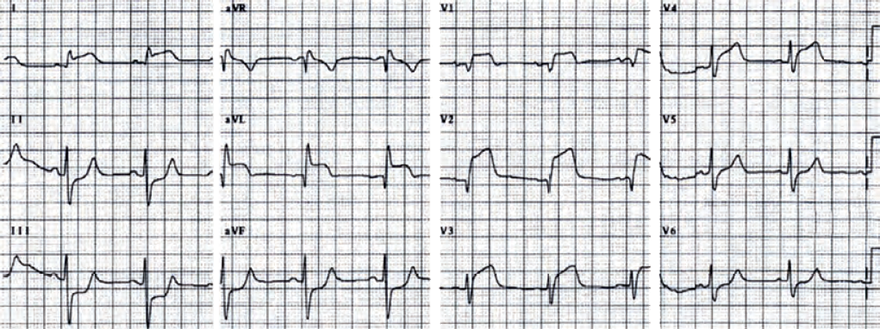
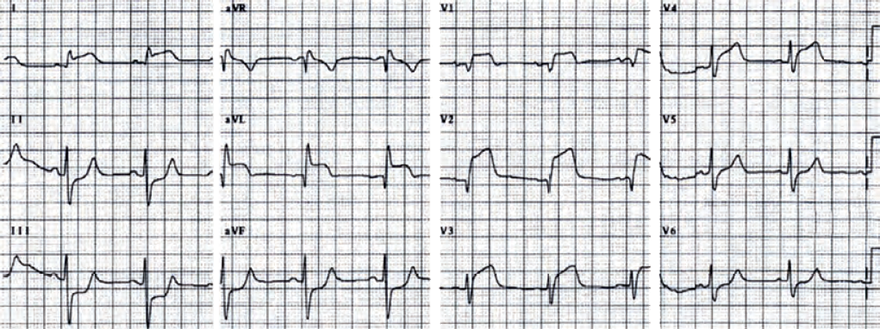
NSTEMI Infarction
|
|
Ischemia Post-Ergometry
|
|
|
Unstable Angina Pectoris
|
|
|
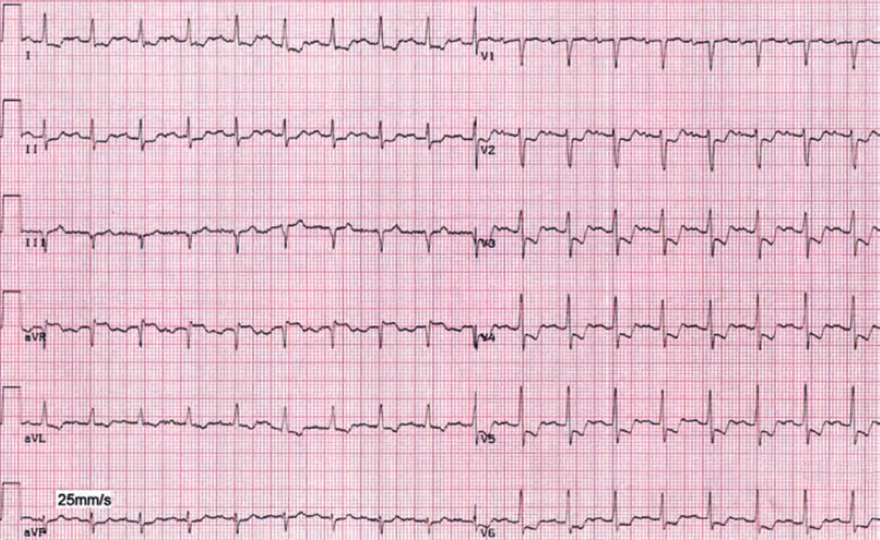
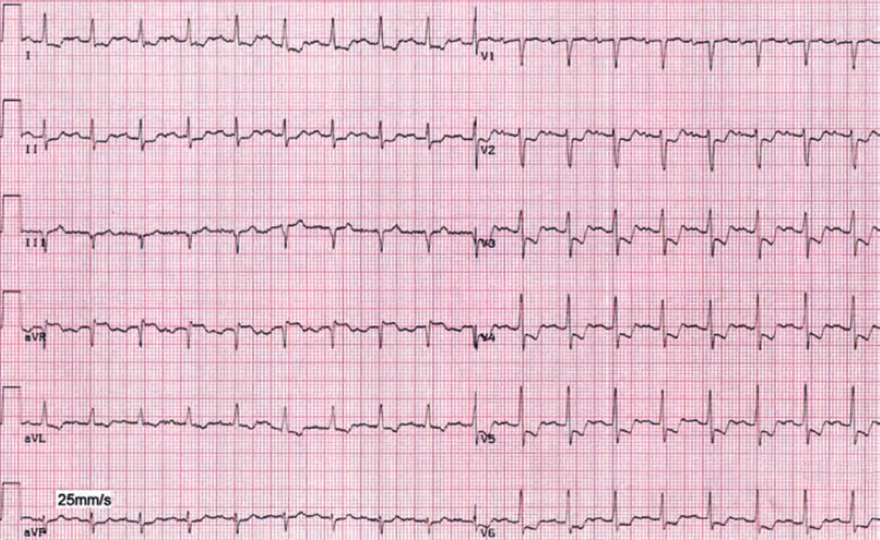
Acute STEMI of the Anterior Wall
|
|
Sources