Home /
Differential Diagnosis of SVT
Differential diagnosis (DDx) of supraventricular tachycardia (SVT)
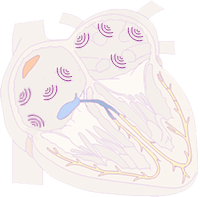
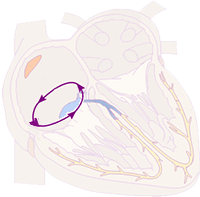
Supraventricular Tachycardia (SVT)
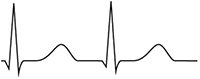
- SVT is a tachycardia (heart rate > 100/min.) with narrow QRS complexes (<0.12s)
- Impulses originate in supraventricular areas (above the bifurcation of the His bundle)
- Impulses can originate via 3 mechanisms:
- Increased automaticity
- Triggering activity
- Re-entry
- The key feature of SVT is narrow QRS complexes (<0.12s)
- The key feature of ventricular tachycardia is wide QRS complexes (≥0.12s)
- Because impulses originate in the ventricles
- Exceptions include 2 narrow-complex ventricular tachycardias (VT):
Paroxysmal SVT
- Paroxysmal SVT is one that starts suddenly and ends suddenly
- It lasts for a few seconds to hours
- The patient experiences palpitations (heart pounding) during the SVT episode
- Paroxysm of SVT can be terminated by:
Paroxysmal SVT
Prevalence of Paroxysmal SVT

- Paroxysmal SVT primarily affects women
- The term paroxysmal SVT only includes:
- In the classification of atrial fibrillation
- The term "paroxysmal atrial fibrillation" is used
- Not paroxysmal SVT
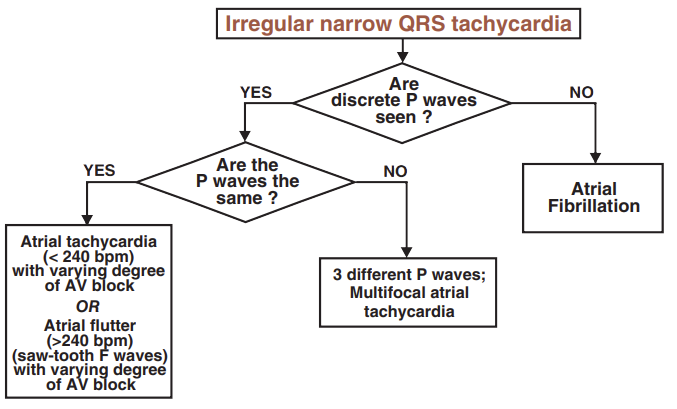
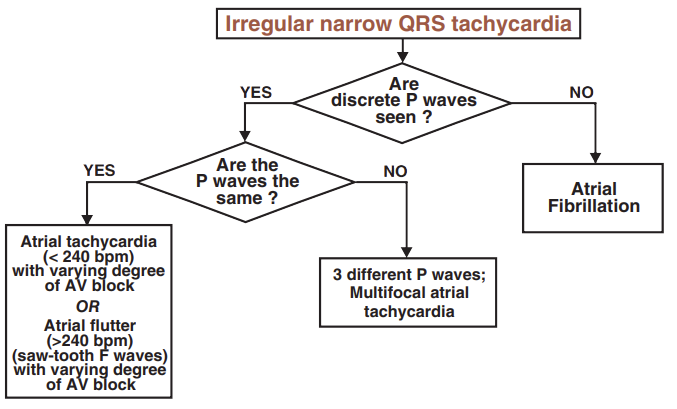
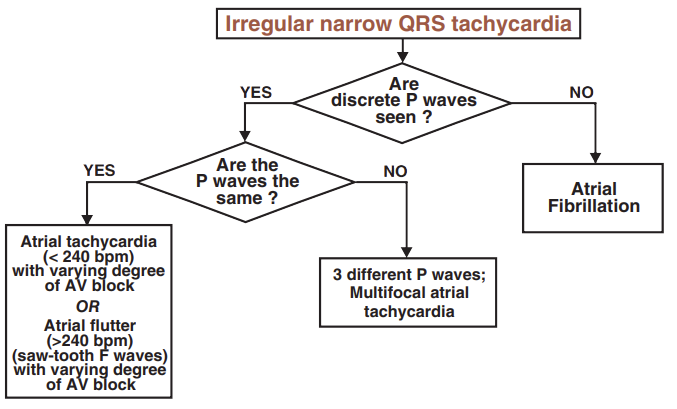
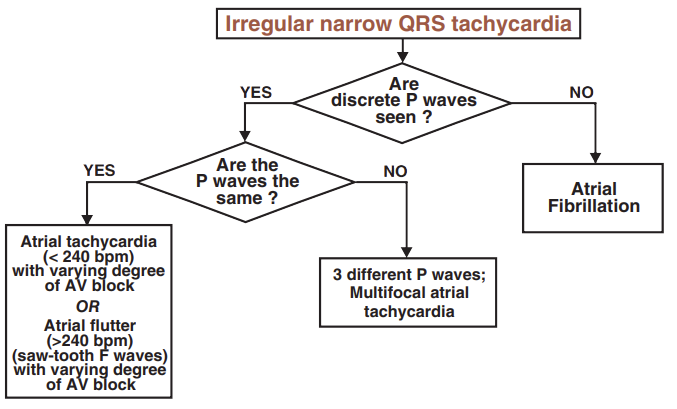
Irregular SVT (Differential Diagnosis)
- Supraventricular tachycardia (SVT) is divided into
- Irregular SVT (simple EKG diagnosis)
- Regular SVT (complex EKG diagnosis)
- Differential diagnosis of SVT uses diagnostic algorithms
Irregular SVT (Differential Diagnosis)
- Atrial Tachycardia
- The impulse originates from a single focus in the atria
- The focus generates impulses with a frequency of < 240/min.
- Atrial Flutter
- The impulse circulates via macro-reentry in the atria with a frequency of > 240/min. (most commonly 300/min.)
- The frequency of P waves is thus > 240/min. (on the EKG, the characteristic sawtooth waves are observed)
- Impulses pass to the ventricles through the AV junction, which can irregularly block impulses
- This results in an irregular ventricular (QRS) response (Variable AV conduction)
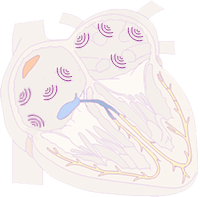
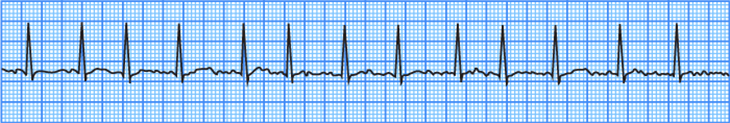
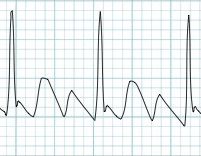
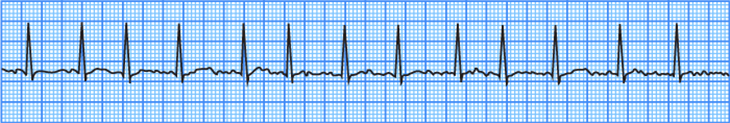
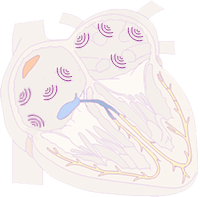
Atrial Fibrillation
- Irregular SVT (QRS complexes are irregular)
- P waves are NOT present (fibrillatory waves are present instead)
- Impulses originate from foci in the atria with a frequency: 350-600/min.
- The AV junction acts as a filter (not every impulse reaches the ventricles)
- Impulses do not generate P waves, impulses that reach the ventricles create QRS
- Mechanism is micro-reentry (most common)
- Atrial Fibrillation
- On EKG, P waves are absent and QRS complexes are irregularly irregular


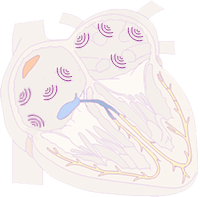
Multifocal Atrial Tachycardia
- Irregular SVT
- Three different P waves are present
- Impulses originate from at least 3 different foci in the atria
- Each impulse creates a P wave, then passes to the ventricles (QRS)
- Each focus (impulse) generates a distinct P wave (different direction of vector)
- Mechanism is increased automaticity (most common)
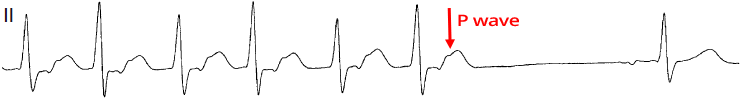
- Multifocal Atrial Tachycardia
- On EKG, there are 3 P waves of different shapes
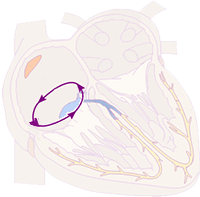
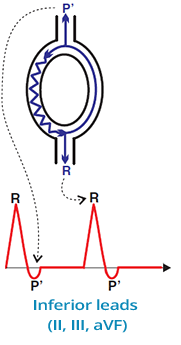
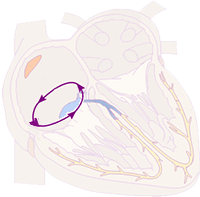
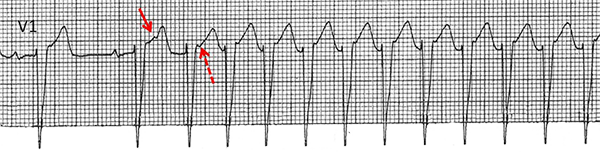
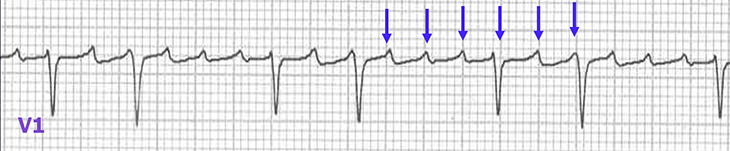
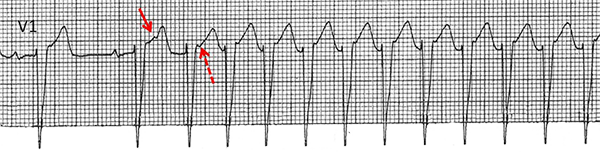
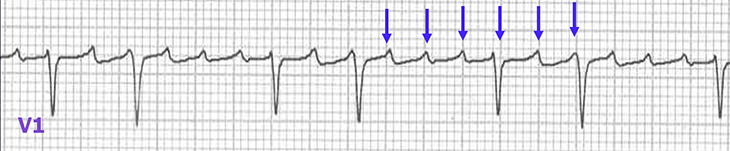
Atrial Flutter
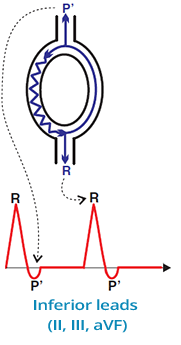
- Irregular SVT
- Sawtooth waves with a frequency of 300/min (>240/min.)
- The impulse circles in the right atrium (Usually around the isthmus with a frequency of 300/min)
- Each rotation in the atrium creates a "sawtooth" impulse
- AV junction acts as a filter (not every impulse passes to the ventricles)
- Impulses pass to the ventricles every second, third, etc.
- Mechanism is macro re-entry (most common)
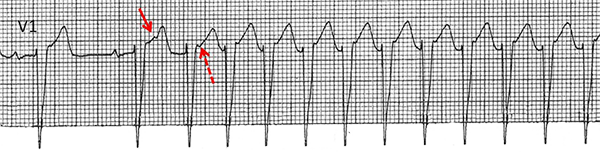
- Atrial Flutter
- On EKG, atrial impulses create characteristic sawtooth waves
- Not every impulse passes through the AV junction to the ventricles
- (On EKG, atrial flutter with varying AV block 2:1 and 4:1)


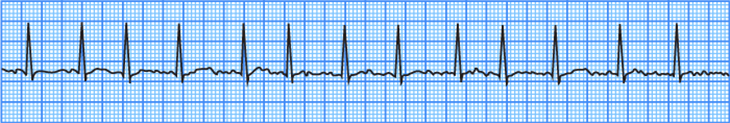
Atrial Tachycardia
- This EKG shows intermittent AV block
- Therefore, the QRS complexes are not in the tachycardia range (>100/min)
- P waves are present with a frequency of 125/min (<240/min)
- If some P waves were blocked, it would create an irregular SVT
- However, this is very rare for atrial tachycardia
- Impulses originate from an ectopic single focus in the atrium (outside the SA node)
- Each impulse creates a P wave, then passes to the ventricles (QRS)
- The P wave from the focus is different from the P wave from the SA node (has a different vector)
- Mechanism is enhanced automaticity (most common)
- Atrial Tachycardia
- On EKG, P waves (different from sinus P waves) are observed
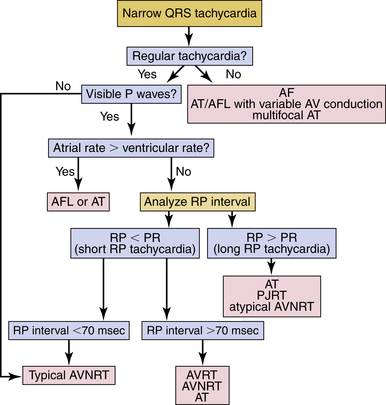
Regular SVT (Differential Diagnosis)
- Diagnosing regular SVT is more complex
- For diagnosing regular SVT, it is ideal to:
- Have older EKGs with sinus rhythm (without SVT)
- During sinus rhythm, look for delta waves (delta waves are associated with AVRT)
- Have the EKG capture the beginning and end of SVT
- Determine if the SVT is paroxysmal
- Observe the response of regular SVT to carotid sinus massage and Adenosine

Regular SVT (Differential Diagnosis)
- In the differential diagnosis of regular SVT
- Evaluate the RP and PR intervals
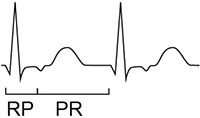
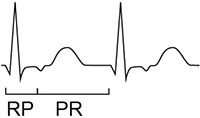
RP and PR Intervals

- Assessed when conduction to the ventricles is 1:1 (P:QRS)
- RP interval (Start of QRS - Start of P wave)
- PR interval (Start of P wave - Start of QRS)
- Intervals are used for differential diagnosis of regular SVT
- SVT with a short RP interval (RP < PR)
- SVT with a long RP interval (RP > PR)
SVT with Short RP Interval (RP < PR)
- Referred to as Short RP tachycardia
- Also includes regular SVT without P waves
- In differential diagnosis, the length of the RP interval is also measured
Without P wave

RP < 90ms
RP > 90ms
SVT with Long RP Interval (RP > PR)
- Referred to as Long RP Tachycardia

RP > PR
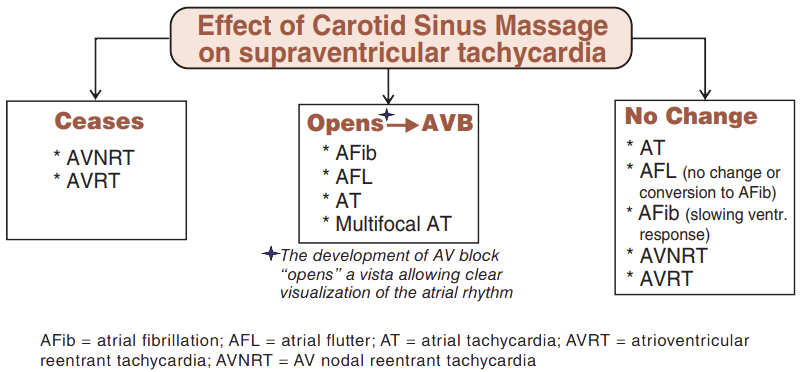
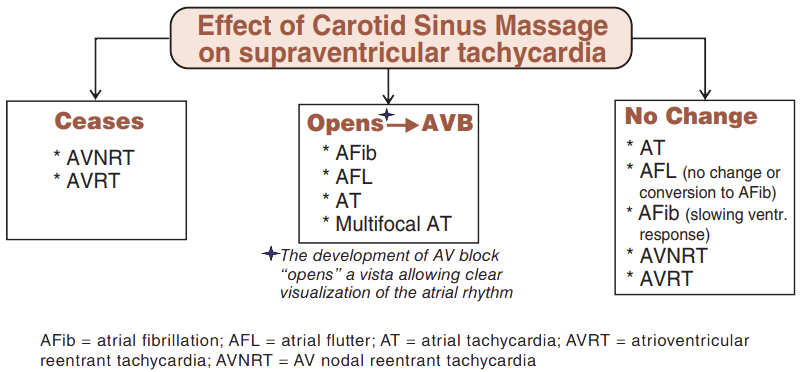
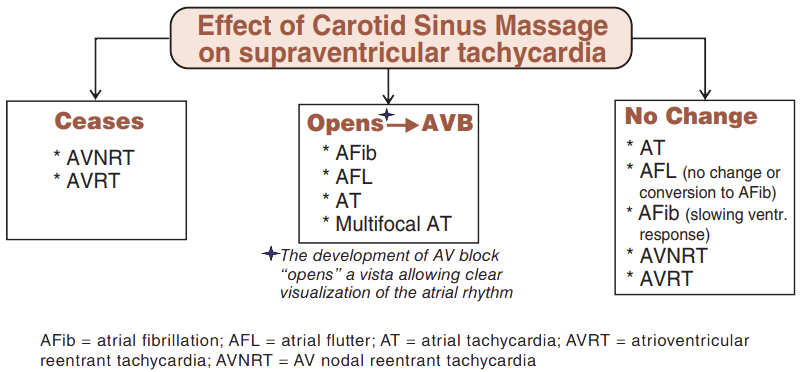
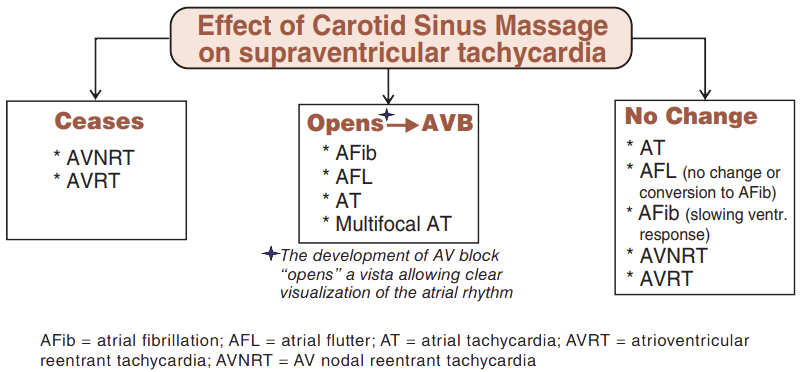
Carotid Sinus Massage
- Slows down automaticity of the atria (not reentry in the atria)
- Slows down impulse conduction through the AV junction
- Terminates SVT with a reentry mechanism
- Prolongs conduction through the AV junction (refractory period) and the reentry circuit is interrupted
- Terminates regular reentry SVT:
- Response of SVT to carotid sinus massage is only 10%
- (Incorrect massage technique, obese patients, physician experience...)
- Similar effects to sinus massage have adenosine
- Response of SVT to adenosine is 90%
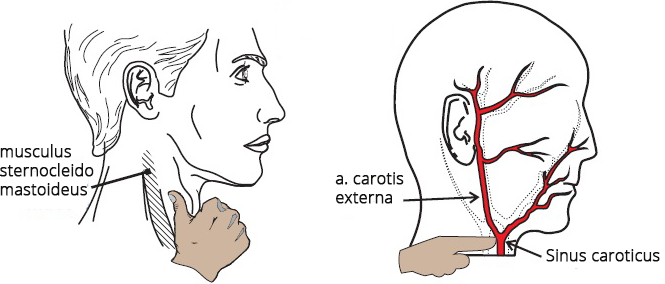
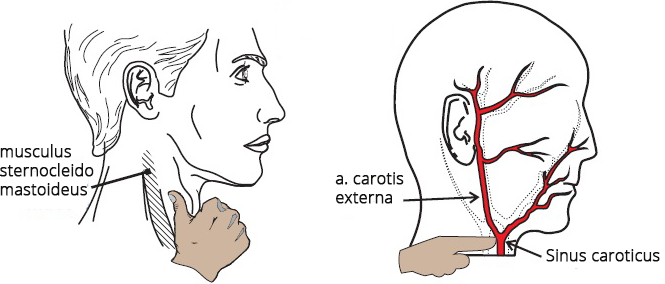
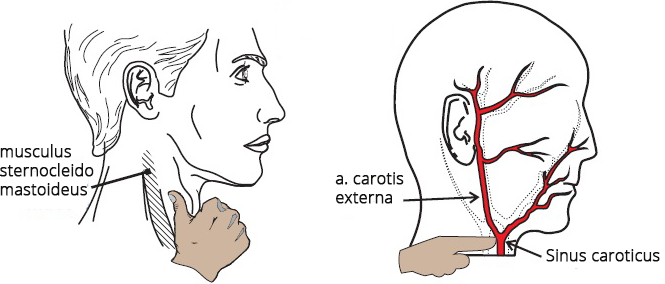
Carotid Sinus Massage Technique
- Carotid Sinus
- Located at the bifurcation of the common carotid artery
- It is a baroreceptor for blood pressure regulation
- When stimulated, it activates the vagus nerve (causing bradycardia and hypotension)
- It is also sensitive to external pressure (neck massage)
- Sinus Location
- In front of the sternocleidomastoid muscle (musculus sternocleidomastoideus)
- At the level of the upper border of the thyroid cartilage
- Palpate the pulsation of the carotid artery
- Massage Technique
- Massage with a circular motion (10-20 seconds) applying "appropriate" pressure
- SVT response typically occurs after 5 seconds
- If unsuccessful, repeat the massage on the other side of the neck
- Always massage only one side of the neck (never bilaterally)
- During the massage, the ECG recording is continuously monitored
- It is important to note the termination of SVT (with a P wave or QRS complex?)
- Do not perform the massage if
- There is a bruit over the carotid artery
- Especially in older individuals, there is a risk of stroke if an atherosclerotic plaque is dislodged
- Suspected hypersensitive carotid sinus
- SVT response to carotid sinus massage is only 10%
- Therefore, in some SVTs, it often does not cause any changes
- (Incorrect massage technique, obese patients, physician experience, etc.)
- Adenosine has similar effects to sinus massage
- SVT response to adenosine is 90%

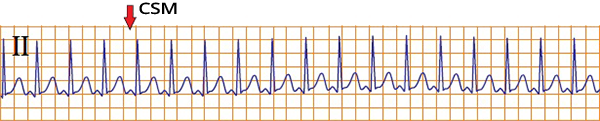
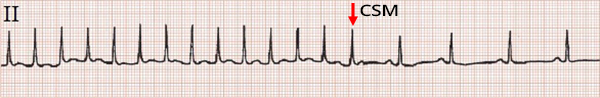
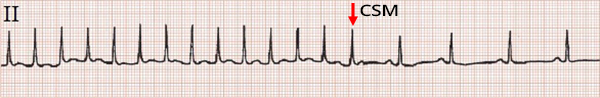
Carotid Sinus Massage and Heart Rate Slowing
- Carotid sinus massage (CSM) slows down the SA node and ectopic foci in the atria in cases of:
- After CSM, there was a decrease in heart rate
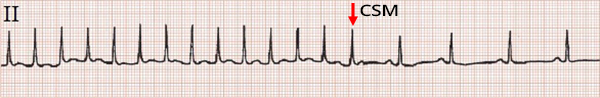
Carotid Sinus Massage and No Decrease in Heart Rate
- Carotid sinus massage (CSM)
- Does not affect reentry in the atria
- Stops reentry only in the AV junction
- No decrease in heart rate after CSM
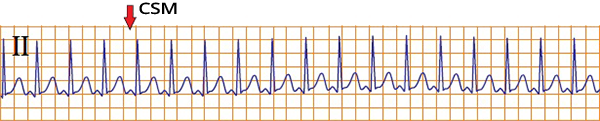
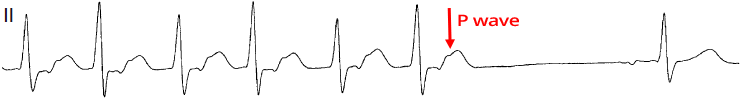
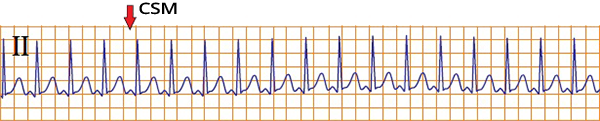
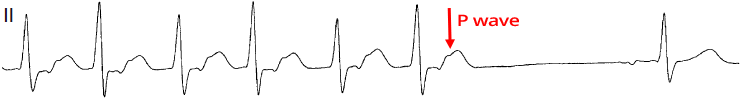
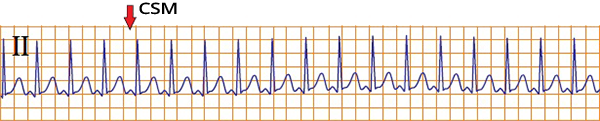
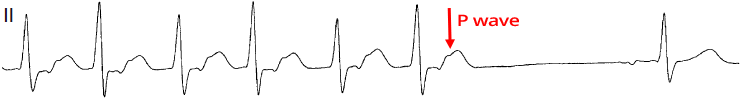
Carotid Sinus Massage and Termination of SVT
- Carotid sinus massage (CSM) terminates SVT with reentry in the AV junction:
- On the ECG, SVT is without P waves
- After CSM, SVT was terminated
- This indicates typical AVNRT
- After the last QRS complex of SVT, a P wave follows
- The patient does not have a delta wave with sinus rhythm (delta wave) (WPW syndrome)

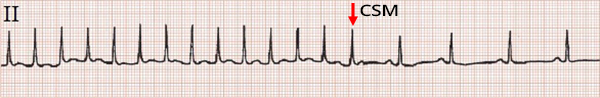
Carotid Sinus Massage and Increased AV Block
- Carotid sinus massage (CSM) increases AV block in SVT:
- After CSM, AV block increased
- Atrial flutter with (2:1) conduction changed to (4:1)
- Flutter waves were unmasked

Carotid Sinus Massage Without Effect
- 10% of SVT respond to carotid sinus massage (CSM)
- 90% of SVT respond to adenosine
- No change in SVT after CSM
- It could be any type of regular SVT
- The patient had a delta wave on EKG with sinus rhythm
Adenosine


- Affects the heart similarly to carotid sinus massage
- The difference lies in the SVT response
- SVT response to
- Carotid sinus massage is only 10%
- Adenosine is 90%
- Dosing of adenosine
- Administer rapidly (within 2 seconds) into a peripheral vein (i.v.)
- Effects last only 10 seconds (short half-life)
- Dosing regimen (6mg -> 1 minute -> 12mg):
- Initial 1st dose is 6mg i.v.
- If SVT does not respond, administer 2nd dose: 12mg i.v. after 1 minute
- If SVT still does not respond, then adenosine is not administered
- Administration of a 3rd dose: 18mg i.v. is controversial
- Contraindicated in Atrial fibrillation with WPW syndrome
- Adenosine blocks the AV junction
- All impulses from the atria then pass to the ventricles
- Results in ventricular fibrillation
Adenosine Test and WPW Syndrome
- In the differential diagnosis of regular SVT
- The presence of a delta wave during sinus rhythm has significant importance
- A delta wave during sinus rhythm almost always indicates AVRT
- 10% of SVTs with a delta wave during sinus rhythm do not have AVRT
- If the accessory pathway is inactive (not part of the SVT mechanism), it is referred to as a bystander "observer"
- Absence of a delta wave (during sinus rhythm) does not exclude AVRT
- The adenosine test is used to uncover a hidden delta wave


Adenosine Test and Delta Wave
- Initially, there is sinus rhythm without delta wave
- 12mg of Adenosine i.v. blocks the AV junction for several seconds
- The impulse starts to propagate through the accessory pathway to the atria
- A delta wave appears on the EKG (black arrow) - WPW syndrome
- The patient has a hidden (inactive) accessory pathway during sinus rhythm
Termination of Regular SVT (with P Wave, QRS?)
- Carotid Sinus Massage (and Adenosine)
- Continuous EKG recording, which captures termination of SVT
- Helps in differential diagnosis of SVT
- Termination of SVT with P Wave (after the last QRS):
- Termination of SVT with QRS Complex:
- If SVT continues after sinus massage (after adenosine)
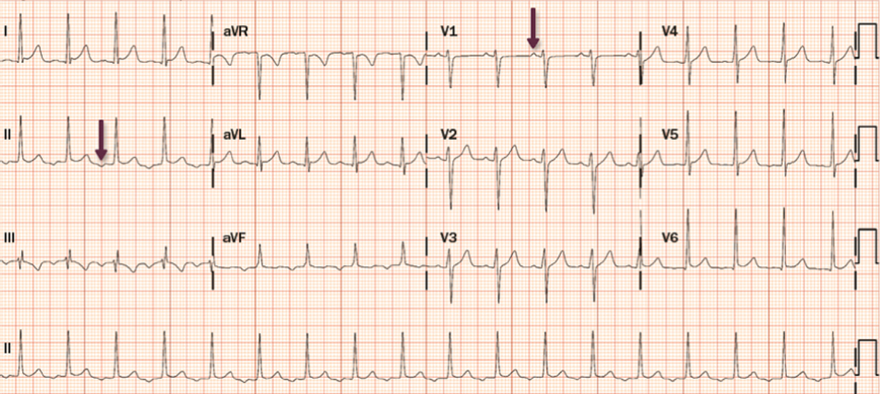
Regular SVT
- QRS Alternans (variation in the height of QRS complexes)
- RP interval > 90ms (the width of the RP interval is estimated from QRS width, without EKG squares)
- After sinus massage, tachycardia was terminated with a P wave
- Patient had a hidden accessory pathway (WPW syndrome) during electrophysiological study
- EKG shows Orthodromic AVRT

Regular SVT
- RP > PR
- After sinus massage, tachycardia was terminated by a QRS complex
- It could again be any of the 3 mentioned SVTs
- Later, SVT recurred (it was a 1-year-old child)
Complete SVT Diagnosis Algorithm
- Complete algorithm for differential diagnosis of SVT (both irregular and regular SVT)
- The algorithm diagnoses SVT based on EKG during SVT
- Does not assess SVT response: to sinus massage, adenosine, termination of SVT (with P wave, QRS?)
- The algorithm is often insufficient and differential diagnosis requires
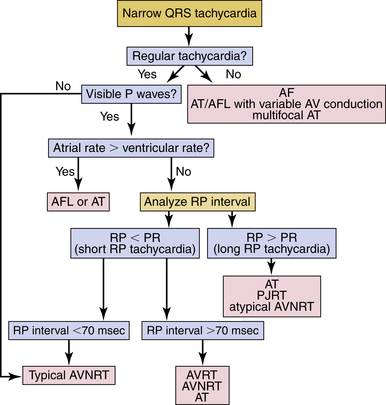
- The most challenging to differentiate are regular SVT:

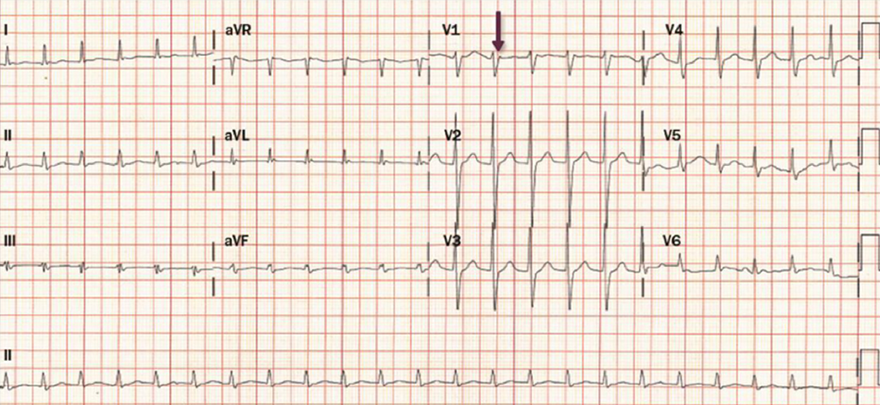
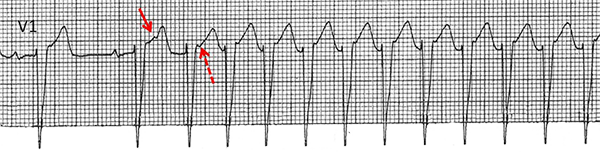
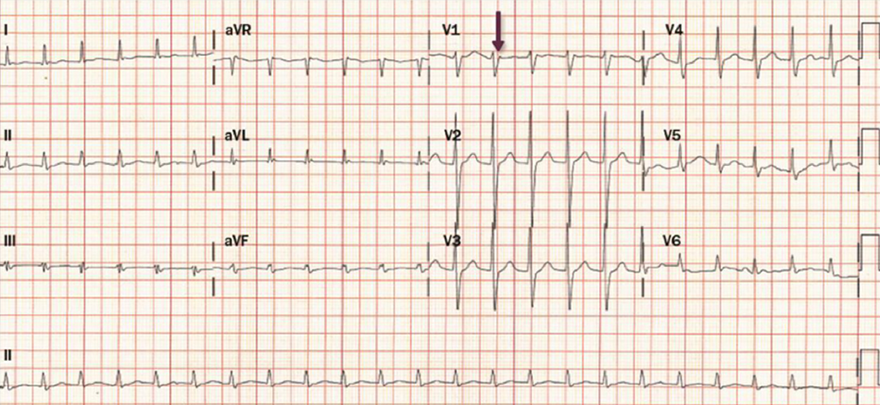
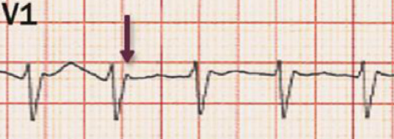
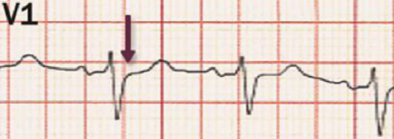
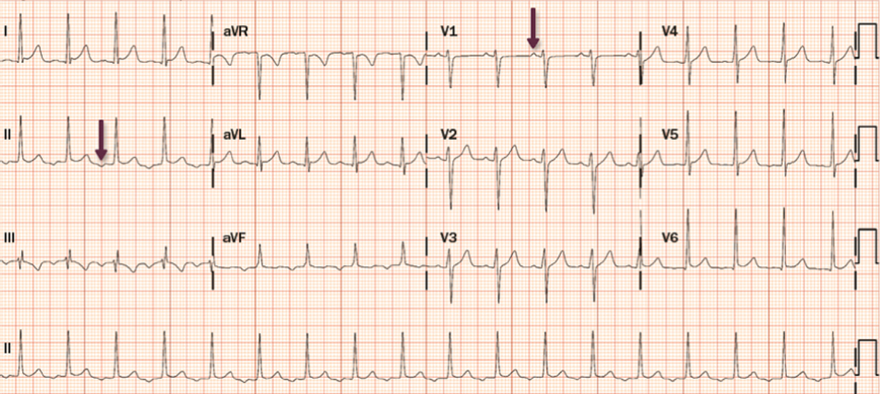
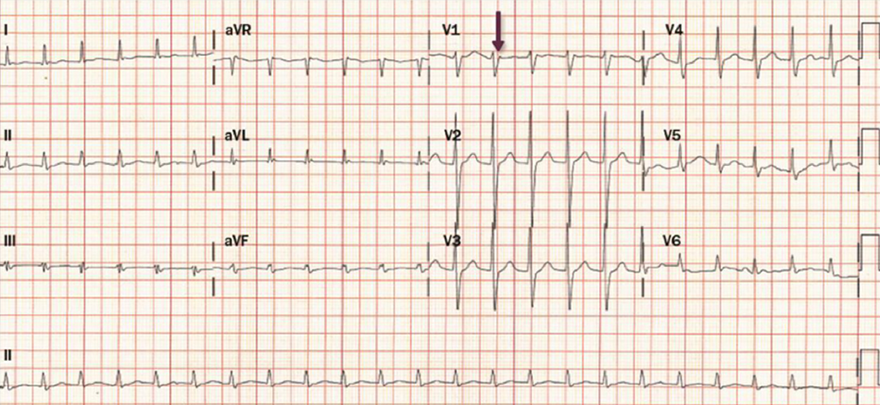
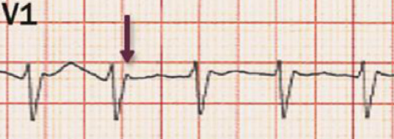
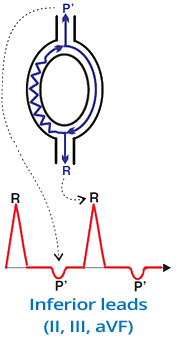
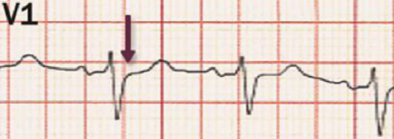
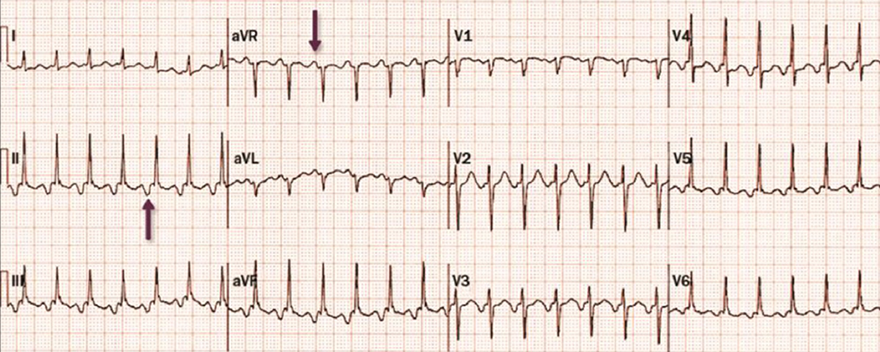
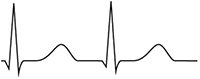
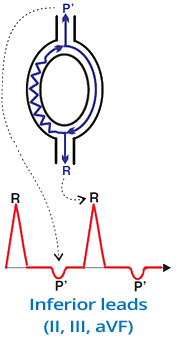
SVT with Short RP Interval (Without P Waves)
- P waves are absent
- Typical AVNRT creates
- Pseudo r' wave (V1) after QRS (arrow)
- Pseudo s wave (II, III, aVF)
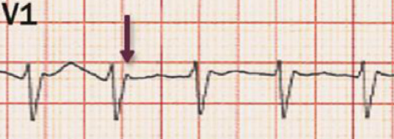
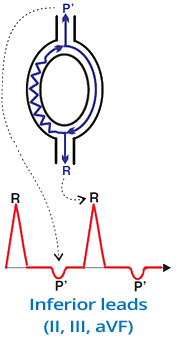
Pseudo r' (V1) in AVNRT
- Indicates typical AVNRT (Slow-Fast)
- Occurs due to retrograde P wave (P')
- Retrograde P wave creates
- Pseudo s' wave in the inferior leads
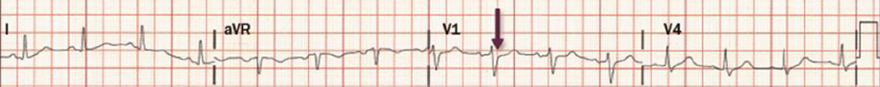
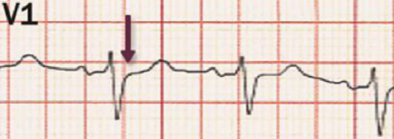
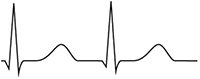
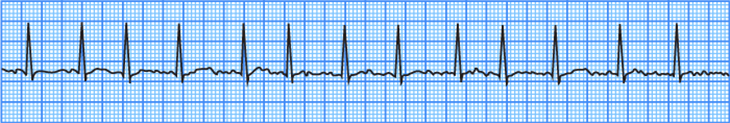
Sinus Rhythm
- This is an ECG from a previous patient
- AVNRT is terminated by carotid sinus massage (adenosine)
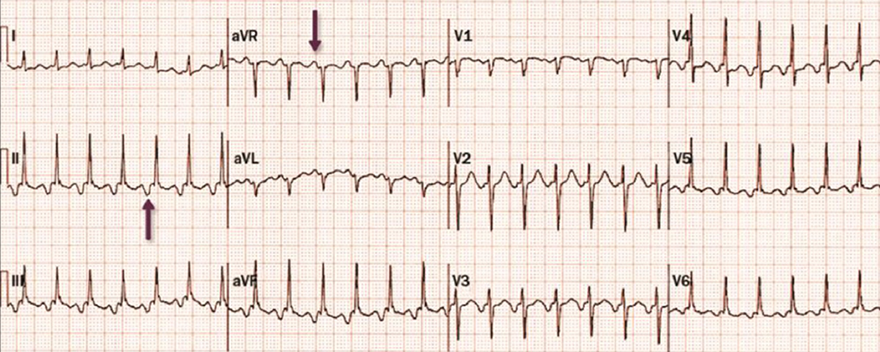
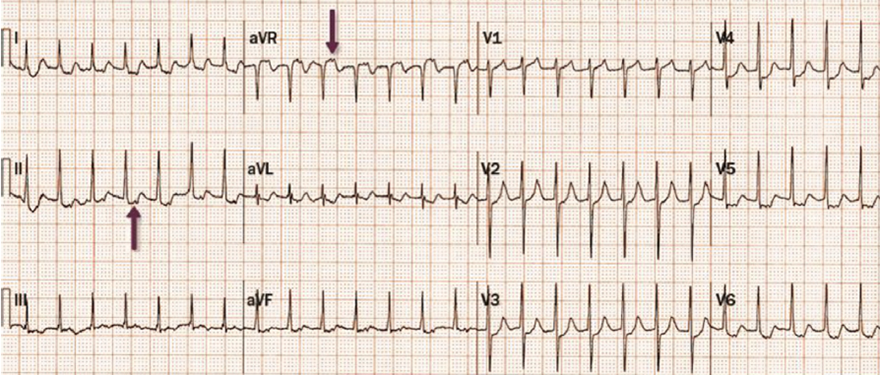
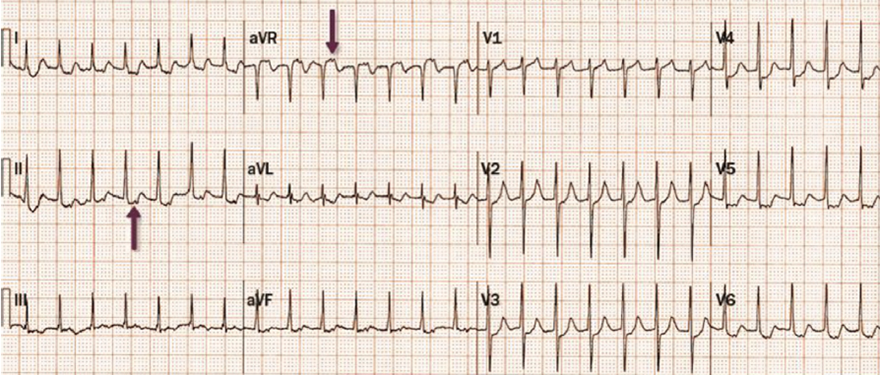
SVT with Long RP Interval (RP > PR)
- The patient is a 30-year-old woman who presented with palpitations
- According to the algorithm, this is an SVT with a long RP interval (RP > PR):
- After administration of adenosine 6mg i.v., conversion to sinus rhythm occurred
- It is not PJRT
- PJRT typically occurs in children under 1 year old
- And recurs after conversion to sinus rhythm
- It is not Atrial Tachycardia
- Atrial Tachycardia does not terminate after adenosine administration
- It is atypical AVNRT (Fast-Slow)
- Retrograde P wave after QRS (II, III, aVF)
- P wave after QRS (aVR)

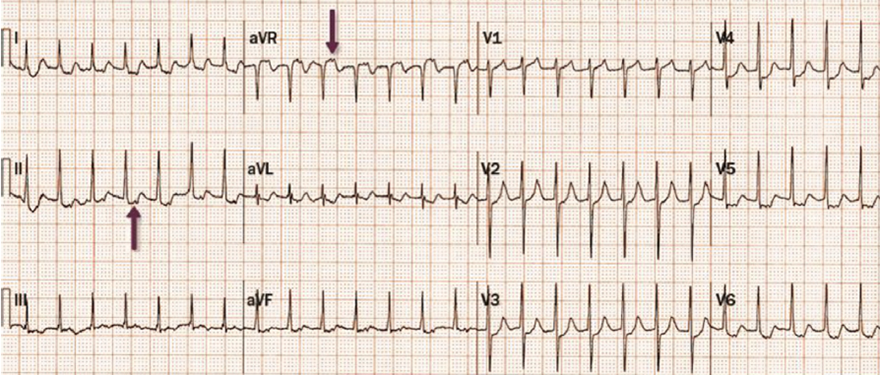
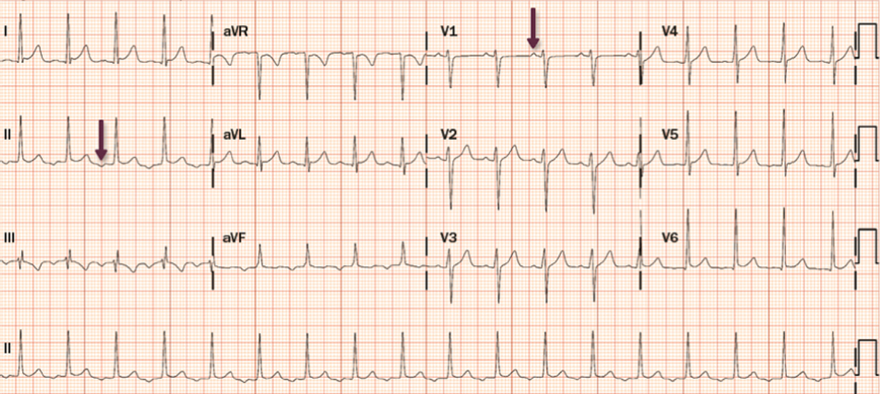
SVT with Short RP Interval (RP > 90ms)
- According to the algorithm, SVT with a short RP interval and RP > 90ms includes:
- After carotid sinus massage, conversion to sinus rhythm occurred
- The patient had a delta wave (which suggests AVRT)
- It is Orthodromic AVRT
- Retrograde P wave after QRS (II, III, aVF)
- P wave after QRS (aVR)
- Delta wave during sinus rhythm

SVT with Long RP Interval (RP > PR)
- According to the algorithm, SVT with a long RP interval (RP > PR) includes:
- SVT did not respond to adenosine
- This excludes reentry mechanisms through the AV junction (AVNRT, PJRT)
- Additionally, the mentioned SVTs most commonly have a heart rate > 150/min.
- This is atrial tachycardia


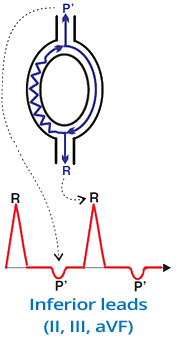
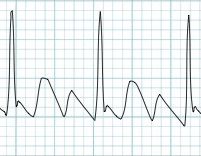
SVT with Long RP Interval (RP > PR)
- The first 2 beats are sinusoidal, then SVT starts (without extrasystole)
- According to the algorithm, SVT with a long RP interval (RP > PR) includes:
- SVT responded to adenosine
- However, after conversion to sinus rhythm, SVT recurred
- Characteristics of permanent junctional reciprocating tachycardia (PJRT) include:
- Heart rate: 120-200/min.
- Occurs mainly in children (under 1 year of age)
- PJRT paroxysms start without extrasystole
- Responds to adenosine
- But often recurs after conversion to sinus rhythm
- Definitive diagnosis is often based on electrophysiological study
Sources
- ECG from Basics to Essentials Step by Step
- litfl.com
- ecgwaves.com
- metealpaslan.com
- medmastery.com
- uptodate.com
- ecgpedia.org
- wikipedia.org
- Strong Medicine
- Understanding Pacemakers

Home /
Differential Diagnosis of SVT
Differential diagnosis (DDx) of supraventricular tachycardia (SVT)
Supraventricular Tachycardia (SVT)
- SVT is a tachycardia (heart rate > 100/min.) with narrow QRS complexes (<0.12s)
- Impulses originate in supraventricular areas (above the bifurcation of the His bundle)
- Impulses can originate via 3 mechanisms:
- Increased automaticity
- Triggering activity
- Re-entry
- The key feature of SVT is narrow QRS complexes (<0.12s)
- The key feature of ventricular tachycardia is wide QRS complexes (≥0.12s)
- Because impulses originate in the ventricles
- Exceptions include 2 narrow-complex ventricular tachycardias (VT):
|
|
Paroxysmal SVT
- Paroxysmal SVT is one that starts suddenly and ends suddenly
- It lasts for a few seconds to hours
- The patient experiences palpitations (heart pounding) during the SVT episode
- Paroxysm of SVT can be terminated by:
Paroxysmal SVT
|
|
Prevalence of Paroxysmal SVT
- Paroxysmal SVT primarily affects women
- The term paroxysmal SVT only includes:
- In the classification of atrial fibrillation
- The term "paroxysmal atrial fibrillation" is used
- Not paroxysmal SVT
|

|
Irregular SVT (Differential Diagnosis)
- Supraventricular tachycardia (SVT) is divided into
- Irregular SVT (simple EKG diagnosis)
- Regular SVT (complex EKG diagnosis)
- Differential diagnosis of SVT uses diagnostic algorithms
Irregular SVT (Differential Diagnosis)
- Atrial Tachycardia
- The impulse originates from a single focus in the atria
- The focus generates impulses with a frequency of < 240/min.
- Atrial Flutter
- The impulse circulates via macro-reentry in the atria with a frequency of > 240/min. (most commonly 300/min.)
- The frequency of P waves is thus > 240/min. (on the EKG, the characteristic sawtooth waves are observed)
- Impulses pass to the ventricles through the AV junction, which can irregularly block impulses
- This results in an irregular ventricular (QRS) response (Variable AV conduction)
|
Atrial Fibrillation
- Irregular SVT (QRS complexes are irregular)
- P waves are NOT present (fibrillatory waves are present instead)
- Impulses originate from foci in the atria with a frequency: 350-600/min.
- The AV junction acts as a filter (not every impulse reaches the ventricles)
- Impulses do not generate P waves, impulses that reach the ventricles create QRS
- Mechanism is micro-reentry (most common)
- Atrial Fibrillation
- On EKG, P waves are absent and QRS complexes are irregularly irregular
|


|
Multifocal Atrial Tachycardia
- Irregular SVT
- Three different P waves are present
- Impulses originate from at least 3 different foci in the atria
- Each impulse creates a P wave, then passes to the ventricles (QRS)
- Each focus (impulse) generates a distinct P wave (different direction of vector)
- Mechanism is increased automaticity (most common)
- Multifocal Atrial Tachycardia
- On EKG, there are 3 P waves of different shapes
|
|
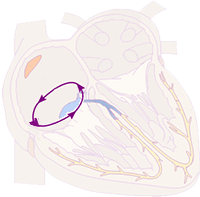
Atrial Flutter
- Irregular SVT
- Sawtooth waves with a frequency of 300/min (>240/min.)
- The impulse circles in the right atrium (Usually around the isthmus with a frequency of 300/min)
- Each rotation in the atrium creates a "sawtooth" impulse
- AV junction acts as a filter (not every impulse passes to the ventricles)
- Impulses pass to the ventricles every second, third, etc.
- Mechanism is macro re-entry (most common)
- Atrial Flutter
- On EKG, atrial impulses create characteristic sawtooth waves
- Not every impulse passes through the AV junction to the ventricles
- (On EKG, atrial flutter with varying AV block 2:1 and 4:1)
|


|
Atrial Tachycardia
- This EKG shows intermittent AV block
- Therefore, the QRS complexes are not in the tachycardia range (>100/min)
- P waves are present with a frequency of 125/min (<240/min)
- If some P waves were blocked, it would create an irregular SVT
- However, this is very rare for atrial tachycardia
- Impulses originate from an ectopic single focus in the atrium (outside the SA node)
- Each impulse creates a P wave, then passes to the ventricles (QRS)
- The P wave from the focus is different from the P wave from the SA node (has a different vector)
- Mechanism is enhanced automaticity (most common)
- Atrial Tachycardia
- On EKG, P waves (different from sinus P waves) are observed
|
Regular SVT (Differential Diagnosis)
- Diagnosing regular SVT is more complex
- For diagnosing regular SVT, it is ideal to:
- Have older EKGs with sinus rhythm (without SVT)
- During sinus rhythm, look for delta waves (delta waves are associated with AVRT)
- Have the EKG capture the beginning and end of SVT
- Determine if the SVT is paroxysmal
- Observe the response of regular SVT to carotid sinus massage and Adenosine

Regular SVT (Differential Diagnosis)
- In the differential diagnosis of regular SVT
- Evaluate the RP and PR intervals
RP and PR Intervals
- Assessed when conduction to the ventricles is 1:1 (P:QRS)
- RP interval (Start of QRS - Start of P wave)
- PR interval (Start of P wave - Start of QRS)
- Intervals are used for differential diagnosis of regular SVT
- SVT with a short RP interval (RP < PR)
- SVT with a long RP interval (RP > PR)
|

|
SVT with Short RP Interval (RP < PR)
- Referred to as Short RP tachycardia
- Also includes regular SVT without P waves
- In differential diagnosis, the length of the RP interval is also measured
|
Without P wave
|

|
RP < 90ms
|
|
RP > 90ms
|
SVT with Long RP Interval (RP > PR)
- Referred to as Long RP Tachycardia

|
RP > PR
|
Carotid Sinus Massage
- Slows down automaticity of the atria (not reentry in the atria)
- Slows down impulse conduction through the AV junction
- Terminates SVT with a reentry mechanism
- Prolongs conduction through the AV junction (refractory period) and the reentry circuit is interrupted
- Terminates regular reentry SVT:
- Response of SVT to carotid sinus massage is only 10%
- (Incorrect massage technique, obese patients, physician experience...)
- Similar effects to sinus massage have adenosine
- Response of SVT to adenosine is 90%
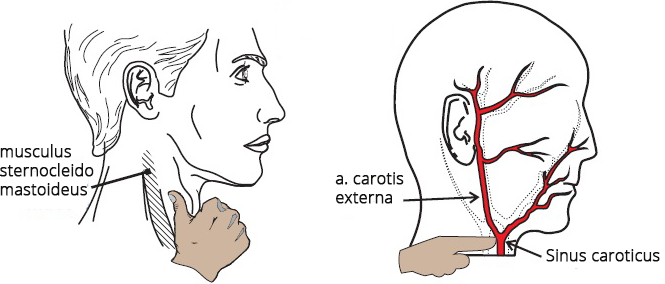
Carotid Sinus Massage Technique
- Carotid Sinus
- Located at the bifurcation of the common carotid artery
- It is a baroreceptor for blood pressure regulation
- When stimulated, it activates the vagus nerve (causing bradycardia and hypotension)
- It is also sensitive to external pressure (neck massage)
- Sinus Location
- In front of the sternocleidomastoid muscle (musculus sternocleidomastoideus)
- At the level of the upper border of the thyroid cartilage
- Palpate the pulsation of the carotid artery
- Massage Technique
- Massage with a circular motion (10-20 seconds) applying "appropriate" pressure
- SVT response typically occurs after 5 seconds
- If unsuccessful, repeat the massage on the other side of the neck
- Always massage only one side of the neck (never bilaterally)
- During the massage, the ECG recording is continuously monitored
- It is important to note the termination of SVT (with a P wave or QRS complex?)
- Do not perform the massage if
- There is a bruit over the carotid artery
- Especially in older individuals, there is a risk of stroke if an atherosclerotic plaque is dislodged
- Suspected hypersensitive carotid sinus
- SVT response to carotid sinus massage is only 10%
- Therefore, in some SVTs, it often does not cause any changes
- (Incorrect massage technique, obese patients, physician experience, etc.)
- Adenosine has similar effects to sinus massage
- SVT response to adenosine is 90%

Carotid Sinus Massage and Heart Rate Slowing
- Carotid sinus massage (CSM) slows down the SA node and ectopic foci in the atria in cases of:
- After CSM, there was a decrease in heart rate
Carotid Sinus Massage and No Decrease in Heart Rate
- Carotid sinus massage (CSM)
- Does not affect reentry in the atria
- Stops reentry only in the AV junction
- No decrease in heart rate after CSM
Carotid Sinus Massage and Termination of SVT
- Carotid sinus massage (CSM) terminates SVT with reentry in the AV junction:
- On the ECG, SVT is without P waves
- After CSM, SVT was terminated
- This indicates typical AVNRT
- After the last QRS complex of SVT, a P wave follows
- The patient does not have a delta wave with sinus rhythm (delta wave) (WPW syndrome)

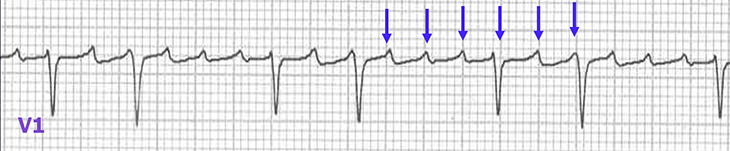
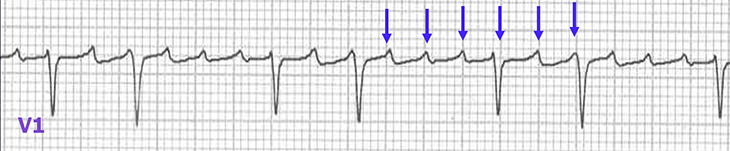
Carotid Sinus Massage and Increased AV Block
- Carotid sinus massage (CSM) increases AV block in SVT:
- After CSM, AV block increased
- Atrial flutter with (2:1) conduction changed to (4:1)
- Flutter waves were unmasked

Carotid Sinus Massage Without Effect
- 10% of SVT respond to carotid sinus massage (CSM)
- 90% of SVT respond to adenosine
- No change in SVT after CSM
- It could be any type of regular SVT
- The patient had a delta wave on EKG with sinus rhythm
Adenosine
- Affects the heart similarly to carotid sinus massage
- The difference lies in the SVT response
- SVT response to
- Carotid sinus massage is only 10%
- Adenosine is 90%
- Dosing of adenosine
- Administer rapidly (within 2 seconds) into a peripheral vein (i.v.)
- Effects last only 10 seconds (short half-life)
- Dosing regimen (6mg -> 1 minute -> 12mg):
- Initial 1st dose is 6mg i.v.
- If SVT does not respond, administer 2nd dose: 12mg i.v. after 1 minute
- If SVT still does not respond, then adenosine is not administered
- Administration of a 3rd dose: 18mg i.v. is controversial
- Contraindicated in Atrial fibrillation with WPW syndrome
- Adenosine blocks the AV junction
- All impulses from the atria then pass to the ventricles
- Results in ventricular fibrillation
|


|
Adenosine Test and WPW Syndrome
- In the differential diagnosis of regular SVT
- The presence of a delta wave during sinus rhythm has significant importance
- A delta wave during sinus rhythm almost always indicates AVRT
- 10% of SVTs with a delta wave during sinus rhythm do not have AVRT
- If the accessory pathway is inactive (not part of the SVT mechanism), it is referred to as a bystander "observer"
- Absence of a delta wave (during sinus rhythm) does not exclude AVRT
- The adenosine test is used to uncover a hidden delta wave

|
Adenosine Test and Delta Wave
- Initially, there is sinus rhythm without delta wave
- 12mg of Adenosine i.v. blocks the AV junction for several seconds
- The impulse starts to propagate through the accessory pathway to the atria
- A delta wave appears on the EKG (black arrow) - WPW syndrome
- The patient has a hidden (inactive) accessory pathway during sinus rhythm
|

|
Termination of Regular SVT (with P Wave, QRS?)
- Carotid Sinus Massage (and Adenosine)
- Continuous EKG recording, which captures termination of SVT
- Helps in differential diagnosis of SVT
- Termination of SVT with P Wave (after the last QRS):
- Termination of SVT with QRS Complex:
- If SVT continues after sinus massage (after adenosine)
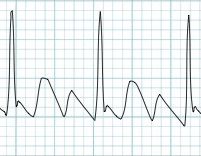
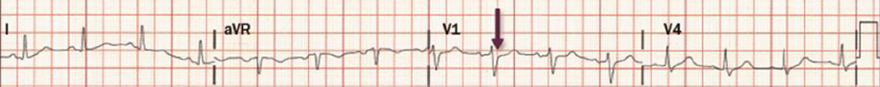
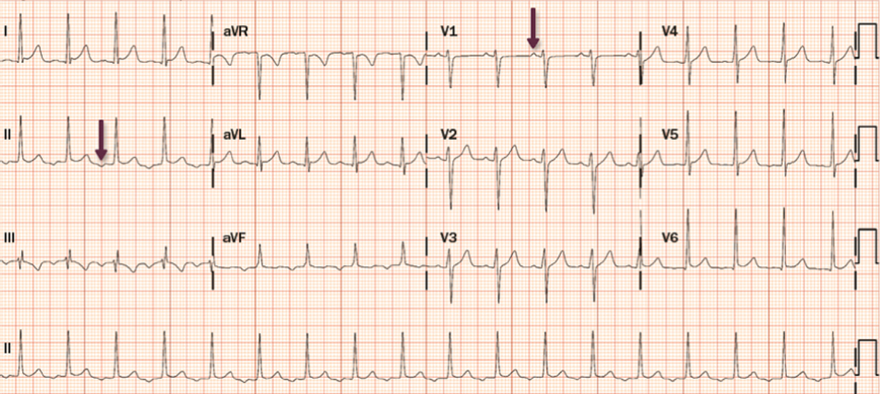
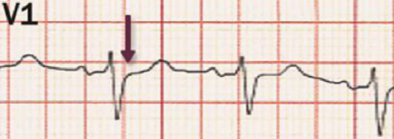
Regular SVT
- QRS Alternans (variation in the height of QRS complexes)
- RP interval > 90ms (the width of the RP interval is estimated from QRS width, without EKG squares)
- After sinus massage, tachycardia was terminated with a P wave
- Patient had a hidden accessory pathway (WPW syndrome) during electrophysiological study
- EKG shows Orthodromic AVRT

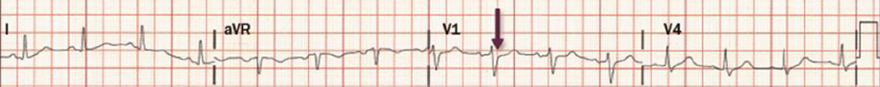
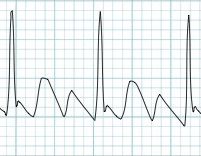
Regular SVT
- RP > PR
- After sinus massage, tachycardia was terminated by a QRS complex
- It could again be any of the 3 mentioned SVTs
- Later, SVT recurred (it was a 1-year-old child)
Complete SVT Diagnosis Algorithm
- Complete algorithm for differential diagnosis of SVT (both irregular and regular SVT)
- The algorithm diagnoses SVT based on EKG during SVT
- Does not assess SVT response: to sinus massage, adenosine, termination of SVT (with P wave, QRS?)
- The algorithm is often insufficient and differential diagnosis requires
- The most challenging to differentiate are regular SVT:
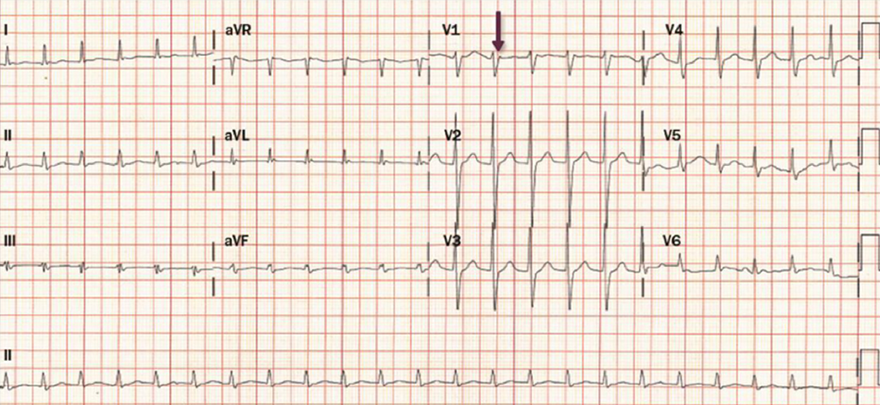
SVT with Short RP Interval (Without P Waves)
- P waves are absent
- Typical AVNRT creates
- Pseudo r' wave (V1) after QRS (arrow)
- Pseudo s wave (II, III, aVF)
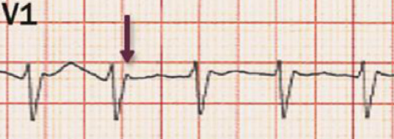
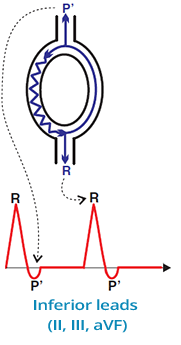
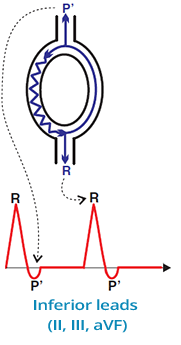
Pseudo r' (V1) in AVNRT
- Indicates typical AVNRT (Slow-Fast)
- Occurs due to retrograde P wave (P')
- Retrograde P wave creates
- Pseudo s' wave in the inferior leads
|

|
|
Sinus Rhythm
- This is an ECG from a previous patient
- AVNRT is terminated by carotid sinus massage (adenosine)
|
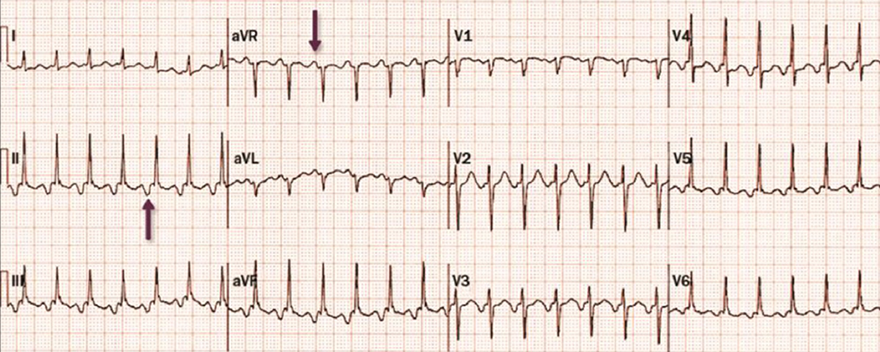
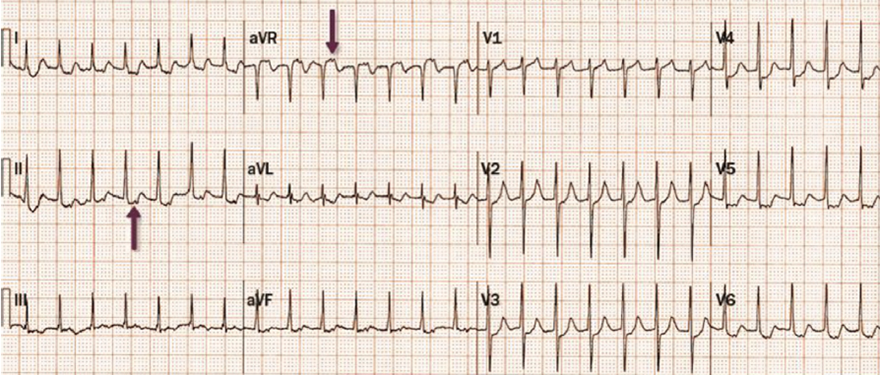
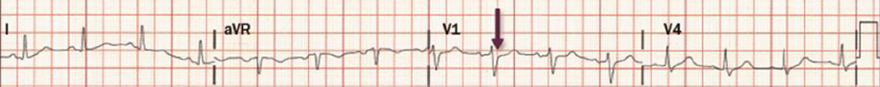
SVT with Long RP Interval (RP > PR)
- The patient is a 30-year-old woman who presented with palpitations
- According to the algorithm, this is an SVT with a long RP interval (RP > PR):
- After administration of adenosine 6mg i.v., conversion to sinus rhythm occurred
- It is not PJRT
- PJRT typically occurs in children under 1 year old
- And recurs after conversion to sinus rhythm
- It is not Atrial Tachycardia
- Atrial Tachycardia does not terminate after adenosine administration
- It is atypical AVNRT (Fast-Slow)
- Retrograde P wave after QRS (II, III, aVF)
- P wave after QRS (aVR)
|
|
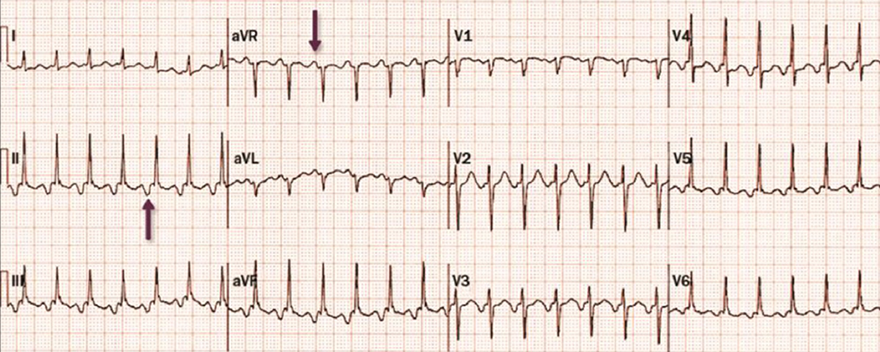
SVT with Short RP Interval (RP > 90ms)
- According to the algorithm, SVT with a short RP interval and RP > 90ms includes:
- After carotid sinus massage, conversion to sinus rhythm occurred
- The patient had a delta wave (which suggests AVRT)
- It is Orthodromic AVRT
- Retrograde P wave after QRS (II, III, aVF)
- P wave after QRS (aVR)
- Delta wave during sinus rhythm
|

|
SVT with Long RP Interval (RP > PR)
- According to the algorithm, SVT with a long RP interval (RP > PR) includes:
- SVT did not respond to adenosine
- This excludes reentry mechanisms through the AV junction (AVNRT, PJRT)
- Additionally, the mentioned SVTs most commonly have a heart rate > 150/min.
- This is atrial tachycardia
|

|

SVT with Long RP Interval (RP > PR)
- The first 2 beats are sinusoidal, then SVT starts (without extrasystole)
- According to the algorithm, SVT with a long RP interval (RP > PR) includes:
- SVT responded to adenosine
- However, after conversion to sinus rhythm, SVT recurred
- Characteristics of permanent junctional reciprocating tachycardia (PJRT) include:
- Heart rate: 120-200/min.
- Occurs mainly in children (under 1 year of age)
- PJRT paroxysms start without extrasystole
- Responds to adenosine
- But often recurs after conversion to sinus rhythm
- Definitive diagnosis is often based on electrophysiological study
|

|
Sources
- ECG from Basics to Essentials Step by Step
- litfl.com
- ecgwaves.com
- metealpaslan.com
- medmastery.com
- uptodate.com
- ecgpedia.org
- wikipedia.org
- Strong Medicine
- Understanding Pacemakers