
|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |

|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |

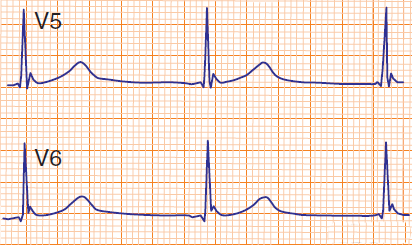
Hypothermia (32°C)

Hypothermia (34°C)

Hypothermia (35°C)

Hypothermia (36°C)

Hypothermia (35°C)

Hypothermia (34°C)

Hypothermia (27°C)

Hypothermia (33°C)

Rapid Onset Hypothermia (31°C)

Hypothermia (32°C)

Hypothermia (35°C)
Hypothermia (36°C)
Sources
Hypothermia
|

|
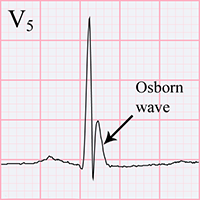
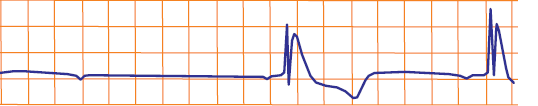
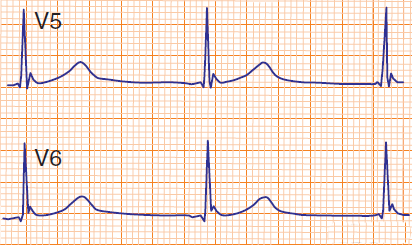
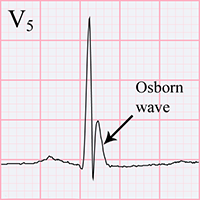
ECG and Hypothermia
|
|
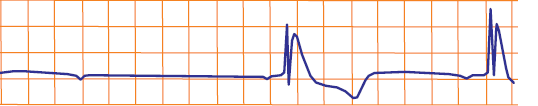
Hypothermia (32°C)

Hypothermia (34°C)

Hypothermia (35°C)

Hypothermia (36°C)

Hypothermia (35°C)

Hypothermia (34°C)

Hypothermia (27°C)

Hypothermia (33°C)

Rapid Onset Hypothermia (31°C)

Hypothermia (32°C)

|
|
|
Hypothermia (35°C)
|
Hypothermia (36°C)
|
Sources