
|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |

|
ECGbook.com Making Medical Education Free for All |
Upload ECG for Interpretation |

Basic Heart Rhythms

Sinus Rhythm


Junctional Rhythm





Junctional Rhythm

Junctional Bradycardia

Junctional Rhythm


Accelerated Junctional Rhythm

Junctional Tachycardia
Junctional Rhythm

Junctional Rhythm

Junctional Rhythm
Junctional Rhythm and Right Bundle Branch Block

Junctional Rhythm

Junctional Bradycardia

Junctional Rhythm and Isorhythmic AV Dissociation
Sources

Basic Heart Rhythms
Junctional Rhythm
|

|
|
Sinus Rhythm
|

|

Junctional Rhythm
|
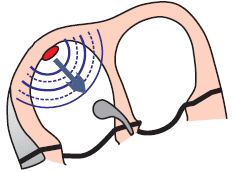
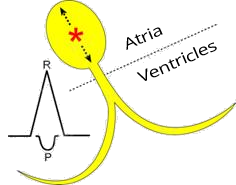
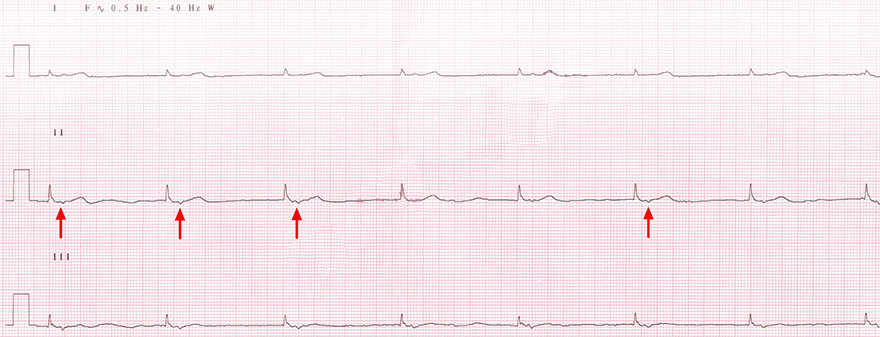
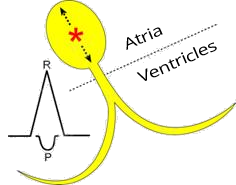
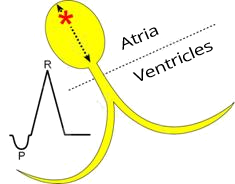
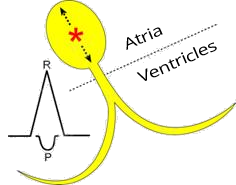
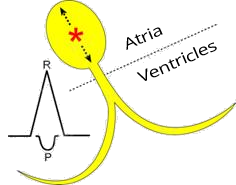
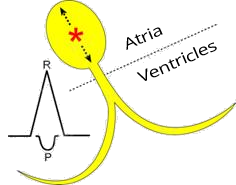
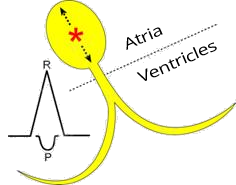
P Wave and Junctional Rhythm
|

|
 |
 |
 |
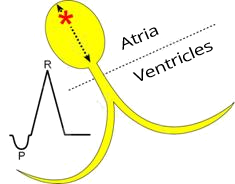
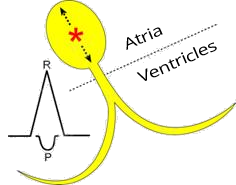
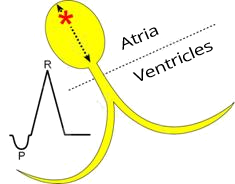
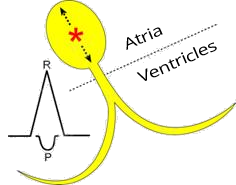
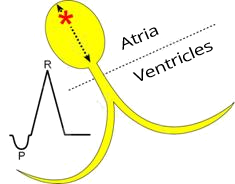
Upper Junctional Rhythm
|
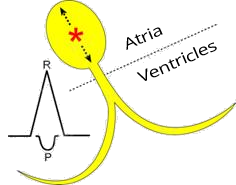
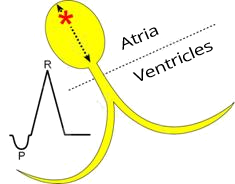
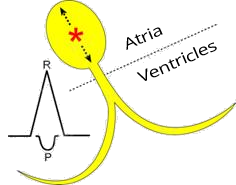
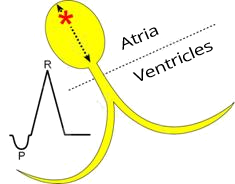
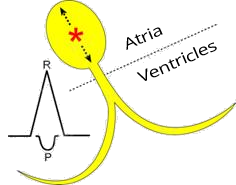
Middle Junctional Rhythm
|
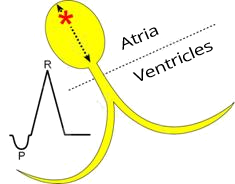
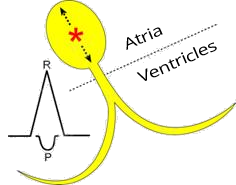
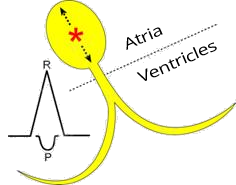
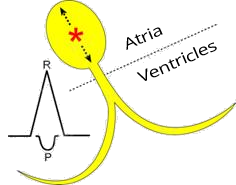
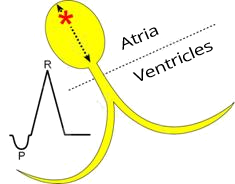
Lower Junctional Rhythm
|
|
Upper Junctional Rhythm
|
|
Middle Junctional Rhythm
|

|
Lower Junctional Rhythm
|
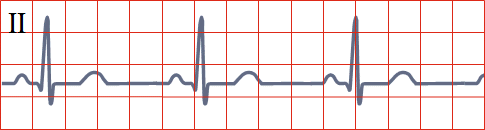
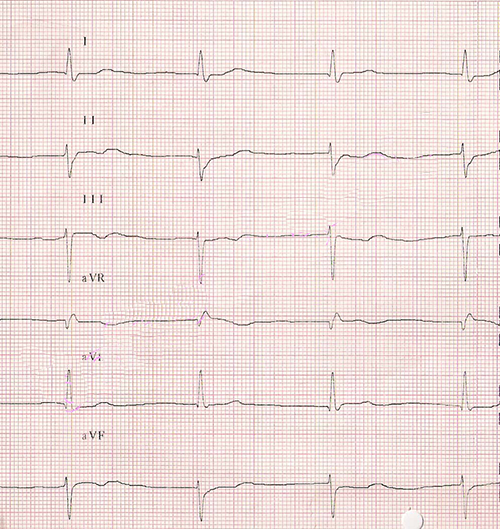
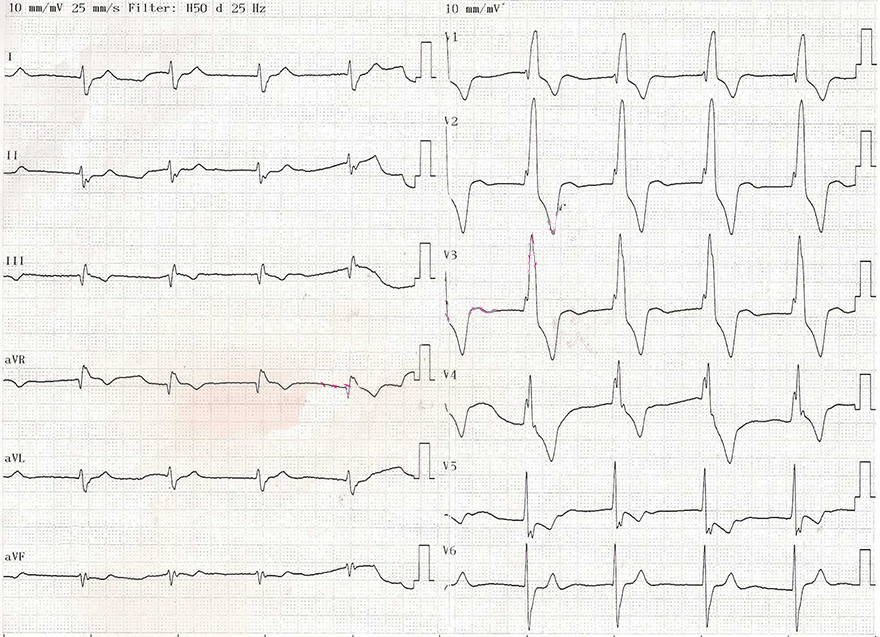
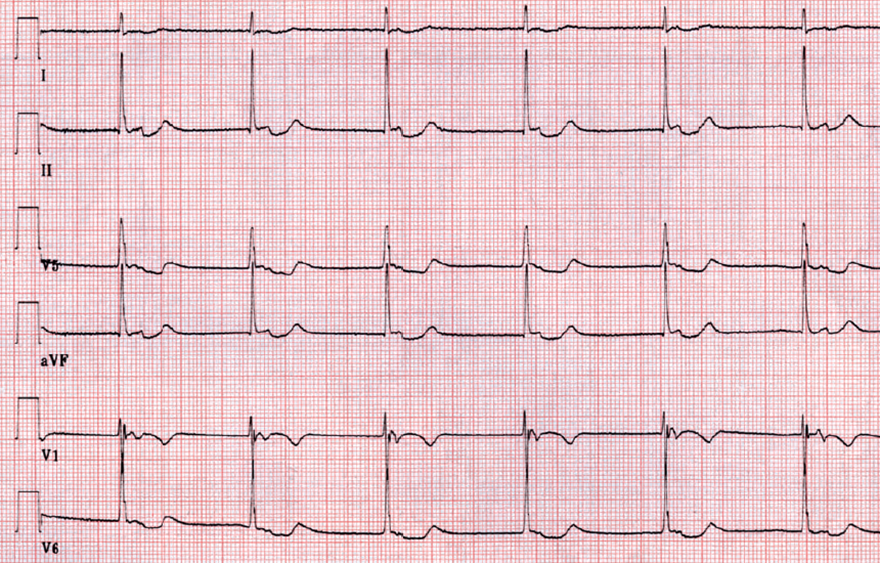
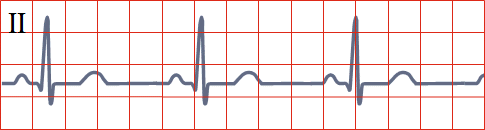
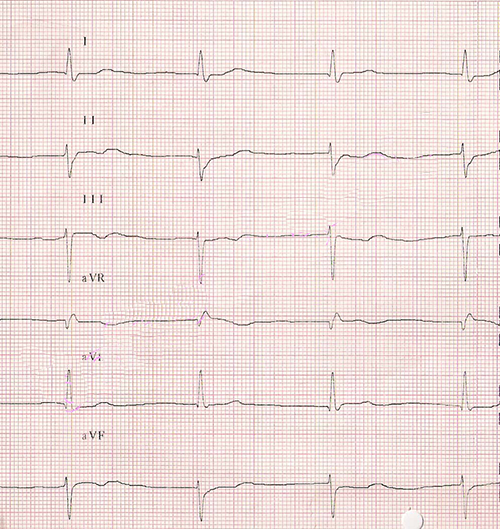
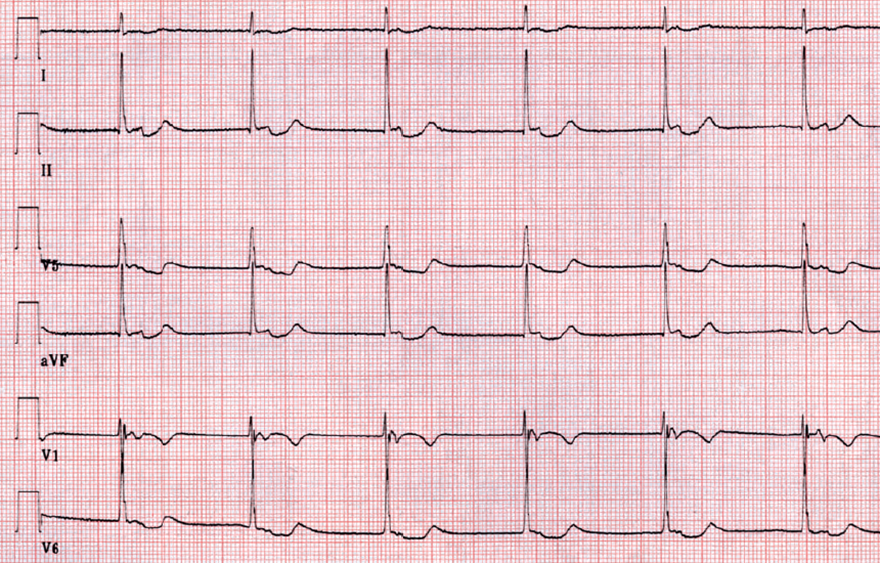
ECG and Junctional Rhythm
|

|

|
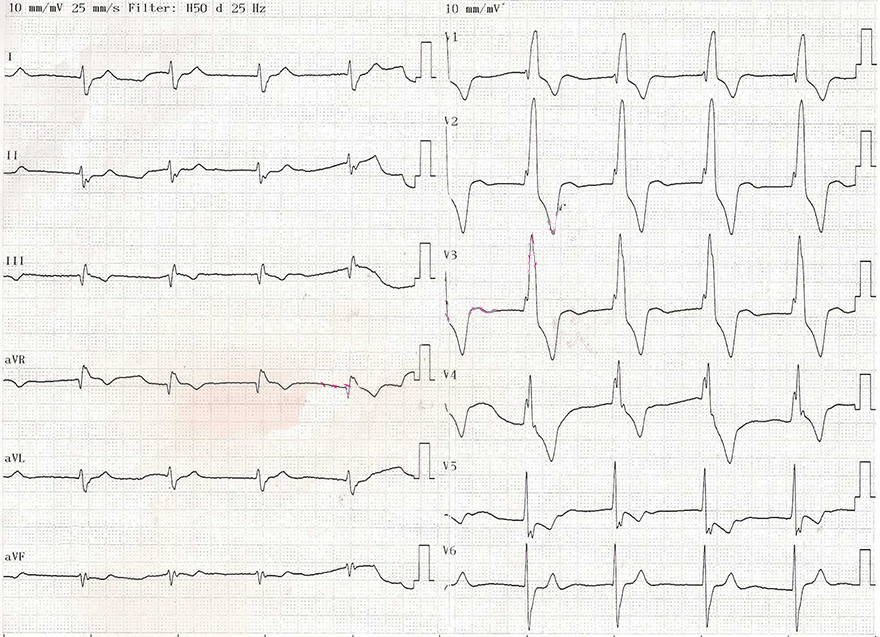
Junctional Rhythm
|
|

|
Junctional Bradycardia
|
|

|
Junctional Rhythm
|
|

|
Accelerated Junctional Rhythm
|

|

|
Junctional Tachycardia
|
|
|
|
|
Junctional Rhythm
|

|
Junctional Rhythm
|
|

|
Junctional Rhythm
|
|
Junctional Rhythm and Right Bundle Branch Block
|
|
|
Junctional Rhythm
|

|

|
|
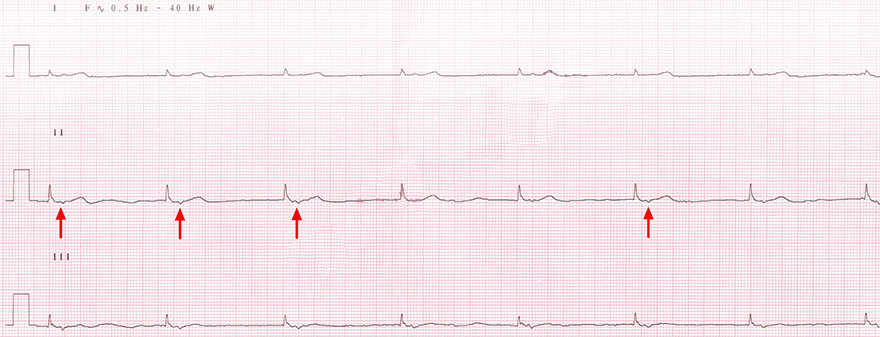
Junctional Bradycardia
|
Junctional Rhythm and Isorhythmic AV Dissociation
|

|
Sources