Home /
Mechanisms of Cardiac Arrhythmias - ECG
Mechanisms of cardiac arrhythmias
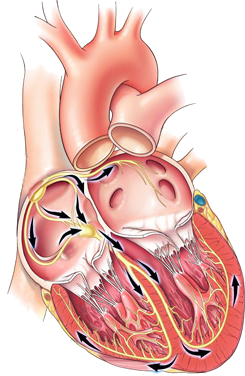
Electrophysiology of the Heart
Arrhythmia
- Physiologically, the heart beats according to the SA node with a frequency of 60-100/min.
- Arrhythmia is a very broad term:
- It fundamentally refers to a disruption of the physiological heart rhythm (a disruption of sinus rhythm)
- The heart beats according to a focus other than the SA node
- or a disruption of the SA node occurs
Mechanisms of Cardiac Arrhythmias
- Arrhythmias occur through 3 mechanisms:
- Automaticity
- Change in normal automaticity
- Abnormal automaticity
- Triggering Activity
- Early afterdepolarization
- Late afterdepolarization
- Reentry
- Anatomical reentry
- Functional reentry
1. Automaticity
- Each cardiomyocyte has the ability for automaticity (spontaneously generate impulses)
- Impulses are generated with the highest frequency in the SA node (primary pacemaker)
- Automaticity can induce arrhythmia through 2 mechanisms:
- Change in normal automaticity
- Abnormal automaticity
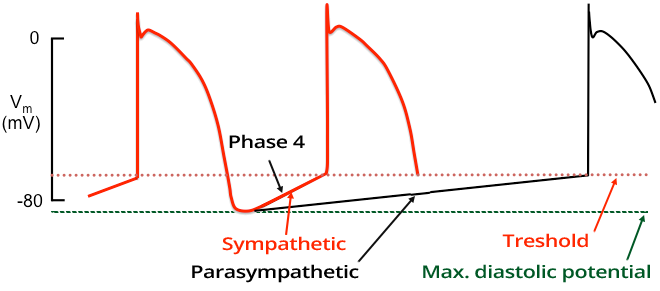
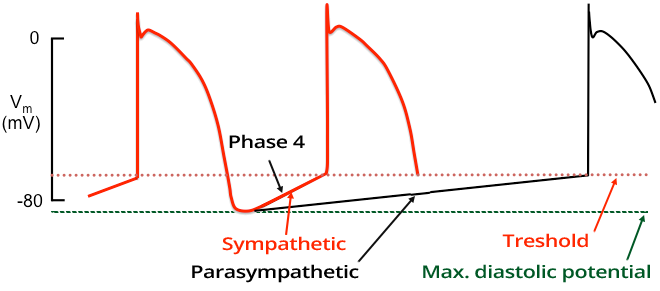
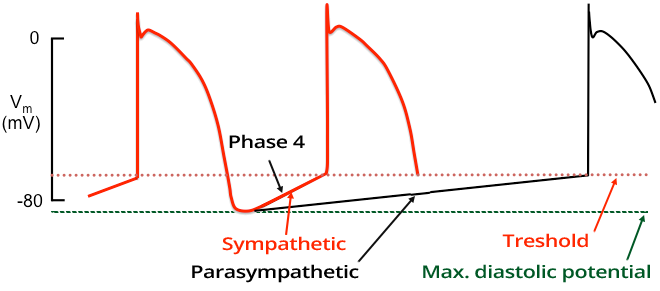
Automaticity and Action Potential
- The rate of automaticity (frequency of impulses) depends on:
- Maximum diastolic potential (the lower value of the action potential)
- Threshold value of the action potential (when exceeded, depolarization is triggered)
- Phase 4 of the action potential (depends on the slope of the curve, a steeper curve reaches the threshold value sooner)
- Automaticity is mainly influenced by the autonomic nervous system (which alters the Phase 4 curve of the AP):
- Arrhythmias due to changes in normal automaticity warm up
- Automaticity increases slowly (frequency slowly increases frequency) and tachycardia does not start with extrasystole
- In reentry, tachycardia starts with extrasystole and the frequency increases from beat (QRS) to beat (QRS)
- A sudden change in frequency is called a paroxysm (a paroxysm starts with extrasystole)
Altered Normal Automaticity
Altered normal automaticity
- It is a change in normal automaticity in cardiac pacemakers:
- Arrhythmias due to altered normal automaticity
Abnormal Automaticity
Abnormal automaticity
- It is activation of automaticity in non-pacemaker areas of the heart
- It involves atrial and ventricular myocardium that does not normally exhibit automaticity under physiological conditions
- It occurs in mineral imbalance, ischemia, low intracellular pH, catecholamine excess
- Arrhythmias due to abnormal automaticity
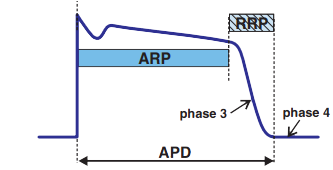
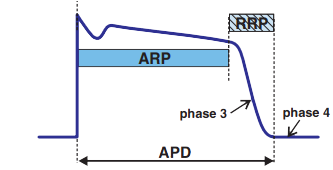
2. Triggered Activity
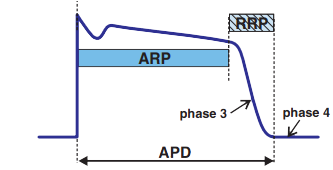
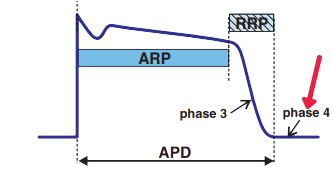
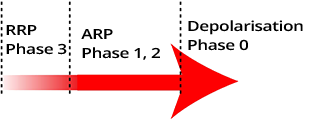
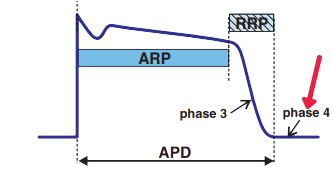
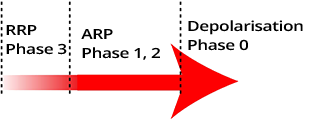
- ARP (Absolute refractory period)
- During ARP, cardiomyocytes do not respond to another impulse
- RRP (Relative refractory period)
- During RRP, cardiomyocytes only respond to a suprathreshold impulse
- Triggered activity means
- that an impulse occurs in a cardiomyocyte
- A premature action potential is generated, which triggers arrhythmia
- Triggered activity can induce arrhythmia through 2 mechanisms:
- Early after-depolarization (occurs during phases 2 and 3)
- Delayed after-depolarization (occurs during phase 4)
Early After-Depolarization
Early afterdepolarization induced Triggered activity

- Depolarization occurs prematurely
- Occurs with prolongation of the action potential
- Arrhythmias associated with early afterdepolarization

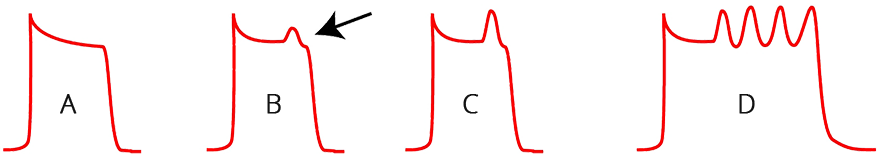
Early After-Depolarization and Torsades de Pointes
- With a prolonged QT interval
- The action potential is prolonged - mainly repolarization (green curve)
- Prolonged repolarization is seen on the ECG during sinus rhythm as a prolonged QT interval
- Early After-Depolarization (EAD)
Early After-Depolarization (Action Potential)
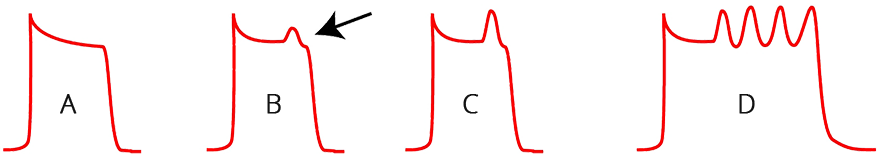
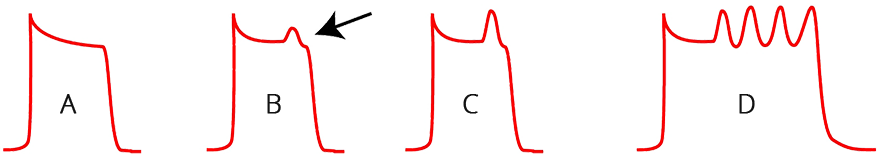
- (A) Normal Action Potential
- The action potential is seen on the ECG as the QT interval
- (B) Early After-Depolarization
- Early after-depolarization occurs in the 2nd phase of the action potential
- No new action potential is generated (because the early after-depolarization did not exceed the "activation threshold")
- (C) Early After-Depolarization and New Action Potential
- (D) Torsades de Pointes (TdP)
- It is academically agreed that TdP is triggered by early after-depolarization
- However, the mechanism during TdP is questionable
Delayed After-Depolarization
Delayed Afterdepolarization Induced Triggered Activity
- Depolarization occurs prematurely
- Risk factors for delayed afterdepolarization include:
- Occurs during tachycardia
- Arrhythmias associated with delayed afterdepolarization

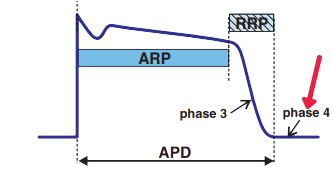
Delayed After-Depolarization (Action Potential)
- (A) Normal Action Potential
- (B) Delayed After-Depolarization
- In the 4th phase of the action potential, delayed after-depolarization occurs
- No new action potential is generated (because the delayed after-depolarization did not exceed the "activation threshold")
- (C) Delayed After-Depolarization and New Action Potential
- Arrhythmia
3. Reentry
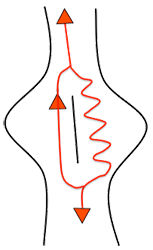
- It is the most common mechanism of arrhythmias
- The impulse (action potential) circulates (most commonly around an anatomical obstacle)
- From the reentry (loop), impulses emerge and activate the myocardium
- Impulses emerge from the reentry exactly like from the SA node in sinus rhythm
- In the past, the reentry mechanism for SVT was referred to by terms:
- Reciprocating tachycardia, Circus movement tachycardia
- These terms are no longer used
Reentry Mechanism
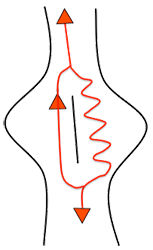
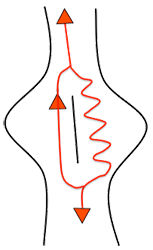
- Reentry is the circling of the same impulse (action potential)
- The impulse must not encounter its own refractory period, as it would cause the reentry to terminate
- The impulse most commonly circles around an anatomical obstacle (such as a scar from a myocardial infarction)

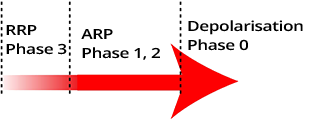
Action Potential
- Impulse in the myocardium of the ventricles is seen on EKG as the QT interval
- After depolarization follows ARP and RRP
- During ARP (Absolute Refractory Period)
- Cardiomyocytes do not respond to a subsequent impulse
- During RRP (Relative Refractory Period)
- Cardiomyocytes respond only to a suprathreshold impulse
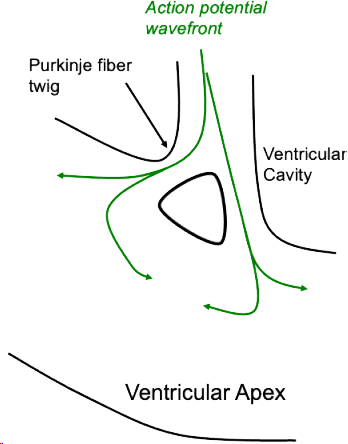
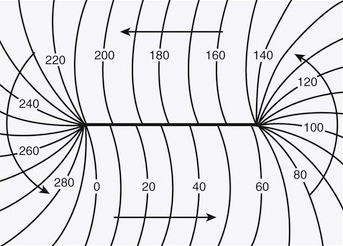
Propagation of Action Potential
- Impulse spreads from the point of origin like an "arrow"
- It actually spreads like throwing a stone into water
- Arrows point outward from the point of origin
- The tip of the arrow represents depolarization
- The tail of the arrow marks the end of RRP (repolarization)

Reentry and Excitation Gap
- The impulse circles most often around an anatomical obstacle
- The tip must not encounter the absolute refractory period
- Reentry would be interrupted
- Excitation gap
- It is the segment between the tip and the end of ARP
- It is an excitability zone within reentry
- It is important for electrophysiological studies
- Used in the diagnosis and treatment of reentry
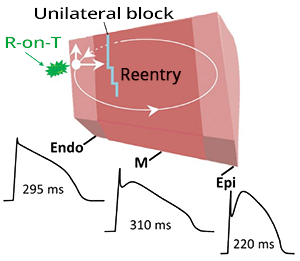
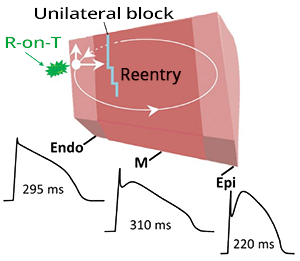
Reentry Formation
- Reentry requires 3 conditions to occur:
- Parallel pathways through which the impulse circulates
- Unidirectional block
- The impulse travels in only one direction through one pathway
- Delayed conduction through one pathway
- During reentry, the impulse slows down, preventing the tip from hitting the refractory period (the tail)
- Reentry is triggered by a atrial or ventricular extrasystole
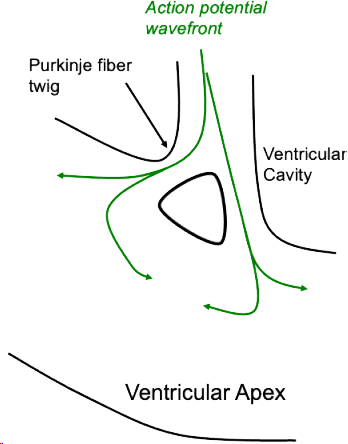
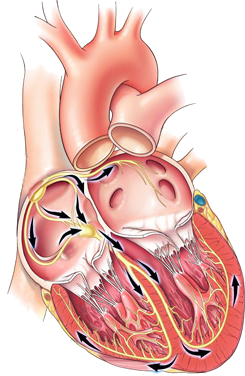
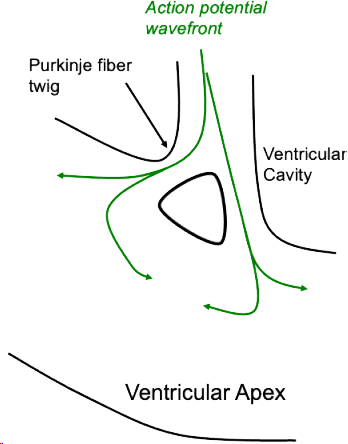
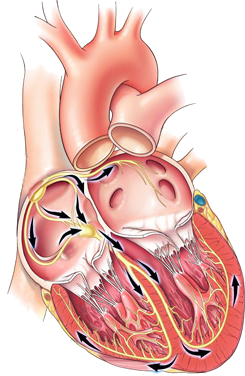
Ventricular Activation via Purkinje Fibers
- The ventricular myocardium is activated by an impulse
- There are 2 parallel pathways
- The fibers are separated by an anatomical obstacle
- It is a physiological obstacle (not a scar from an infarction)
- Behind the obstacle, impulses dissipate and disappear
- The remaining impulses continue to the myocardium
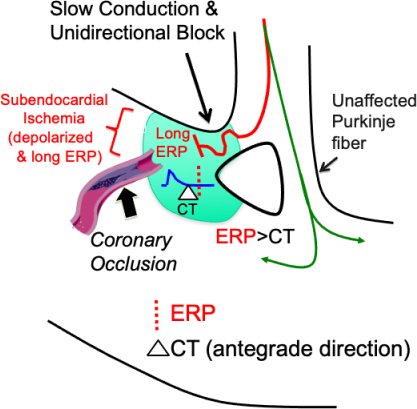
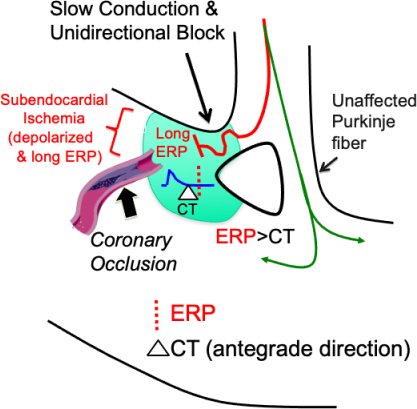
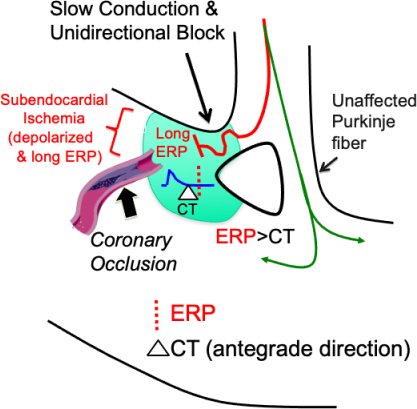
Formation of a Slow Conduction Pathway
- Arterial stenosis causes subendocardial ischemia
- Stenosis is narrowing, occlusion is blockage
- Electrophysiology changes in the ischemic area
- An ischemic myocardium develops
- Impulse then moves to the ventricular myocardium
- only through 1 Purkinje fiber
- The ischemic area blocks the impulse

Start of Reentry
- Reentry begins with a atrial or ventricular extrasystole
- The extrasystole enters the reentry circuit during the excitation gap
- The impulse moves through
- At the end of the slow pathway
- There is no longer anterograde impulse in the ARP
- (ARP - Absolute Refractory Period)
- Retrograde impulse from the slow pathway:
- Begins to circulate in reentry

Reentry
- The impulse circulates
- With each rotation
- Impulses exit the reentry circuit
- and activate the myocardium
- The impulse circulation in reentry
- Is always in the tachycardia zone (frequency > 100/min.)
- Reentry deactivates all other foci in the heart
Classification of Reentry
- Anatomical reentry (most common)
- Functional reentry
- Leading circle reentry
- Anisotropic reentry
- Figure of 8 reentry
- Reflection reentry
- Spiral wave (rotor) reentry
- Phase 2 reentry
Anatomical Reentry

- Anatomical reentry is the most common mechanism of reentry
- The center of reentry is formed by an anatomical obstacle:
- Arrhythmias associated with anatomical reentry:
Functional Reentry
- A functional barrier develops
- It involves an electrophysiological change in the myocardium due to:
- Functional reentry can involve several mechanisms:
- Leading circle reentry
- Anisotropic reentry
- Figure of 8 reentry
- Reflection reentry
- Spiral wave (rotor) reentry
- Phase 2 reentry
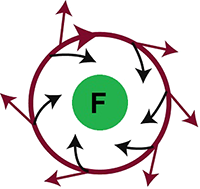
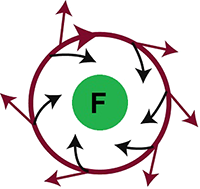
Leading Circle Reentry
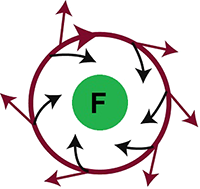
- The center of reentry is formed by a functional barrier (F)
- Impulses from reentry also direct towards the center
- They maintain the center in the absolute refractory period
- The center of reentry is thus non-excitable (it is electrically inactive)
- Arrhythmias associated with Leading Circle Reentry:
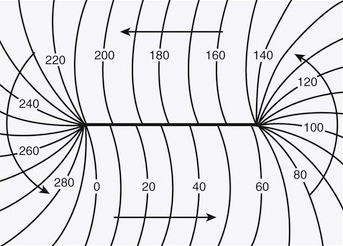
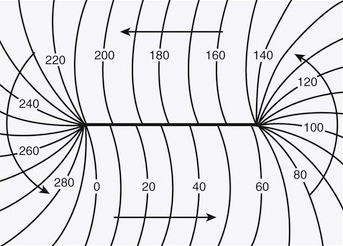
Anisotropic Reentry
- Isotropic conduction
- Has the same conduction properties in all directions
- Anisotropic conduction
- Does not have the same properties in all directions
- Conduction of impulses through myocardium is anisotropic
- Impulse propagation
- In anisotropic reentry
- A refractory line forms in the myocardium
- around which reentry circulates
- The speed of impulse is shown in ms
- Arrhythmias associated with Anisotropic Reentry:
Figure of 8 Reentry

- There are 2 reentry circuits
- Resembling the shape of an eight (8)
- Impulses circulate
- In clockwise and counterclockwise directions
- They share 1 common pathway, which can be separated by:
- Functional or anatomical barriers
- Arrhythmias associated with Figure of 8 Reentry:
Reflection Reentry

- It is an atypical reentry mechanism
- Because the impulse does not circulate in a loop
- The impulse oscillates along a linear axis
- Linear section of the myocardium
- Has electrophysiologically altered area
- At the boundary of the altered myocardium, there is a zone
- The impulse thus oscillates "up and down"
- Along the linear section of the myocardium
- Can occur on an area of 1-2mm2
- Difficult to differentiate from ectopic automaticity
Spiral Wave (Rotor) Reentry

- The central part contains a refractory core
- A wave circulates around the core
- The wave can circulate in 2D or 3D space
- Impulses emanate from the wave, activating the myocardium
- Arrhythmias associated with Spiral Wave (Rotor) Reentry:
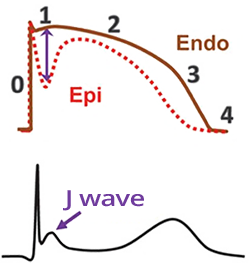
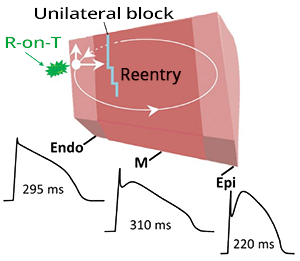
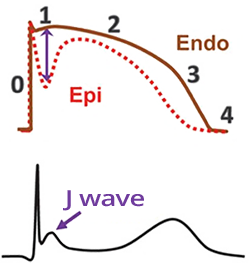
Phase 2 Reentry

- Action Potential (AP) in the myocardial wall
- Differs partially in
- The epicardium
- The mid-myocardium (M-cells)
- The endocardium
- AP also partially differs in
- The right and left ventricles
- Transmural Repolarization Dispersion
- Is the difference in the duration of action potentials (primarily repolarization)
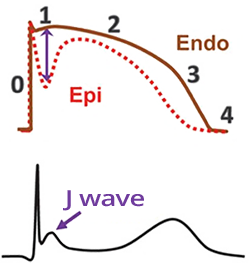
- In the case of functional myocardial disturbance (e.g., ion imbalances, medications, ischemia)
- A difference between phases 1 and 2 of the action potential may occur
- Especially between the endocardium and epicardium
- This appears on the ECG as a change after the QRS complex
- Most commonly seen as a J wave
- Phase 2 reentry
- It is a functional reentry that occurs during a disturbance of phase 2 of the action potential
- Reentry is most commonly triggered by ventricular extrasystole (VES)
- The reentry circuit circulates between the endocardium and epicardium
- The impulse essentially oscillates between the endocardium and epicardium
- This is not a typical circular reentry
J Wave Syndromes
- J wave syndromes: are syndromes with a disturbance in phase 2 of the action potential
- On the ECG, they cause changes after the QRS complex:
- Arrhythmias in Phase 2 reentry
Sources
- ECG from Basics to Essentials Step by Step
- litfl.com
- ecgwaves.com
- metealpaslan.com
- medmastery.com
- uptodate.com
- ecgpedia.org
- wikipedia.org
- Strong Medicine
- Understanding Pacemakers