Home /
Polymorphic Ventricular Tachycardia
Polymorphic ventricular tachycardia
Ventricular Tachycardia
- Ventricular tachycardia (VT) has a ventricular ectopic focus
- The focus generates impulses with a frequency > 100/min.
- Wide QRS complexes (>0.12s) are formed
Basic Classification
- Ventricular tachycardia (VT) consists of at least 3 consecutive ventricular beats
- VT almost always occurs in a structurally damaged heart
- VT by Duration
- Non-sustained VT: at least 3 ventricular QRS complexes lasting < 30s
- Sustained VT: lasts > 30s
- VT by Hemodynamics
- Hemodynamically stable: the patient is hemodynamically stable
- Usually associated with VT with a frequency of < 160/min.
- Hemodynamically unstable: the patient is hemodynamically unstable
- Usually associated with VT with a frequency of > 160/min.
- Not precisely defined, the patient's blood pressure, pulse, and respiratory rate...
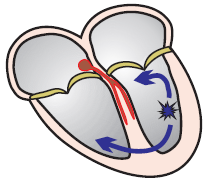
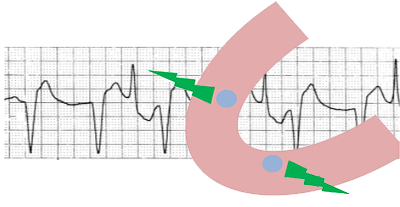
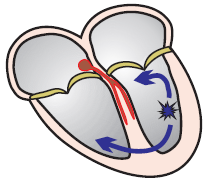
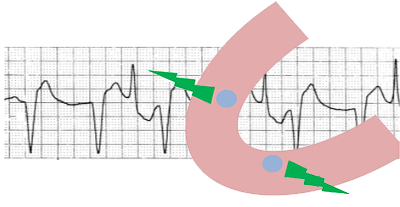
Monomorphic Ventricular Tachycardia
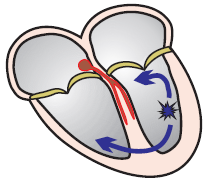
- Monomorphic VT is the most common type of ventricular tachycardia
- Occurs in a structurally damaged heart
- A reentry circuit forms in the scar
- And generates impulses with a frequency of > 100/min.
- All QRS complexes are monomorphic (identical)
- Therefore, it is referred to as monomorphic
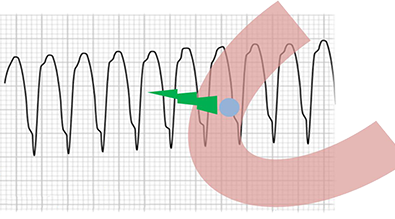
Monomorphic Ventricular Tachycardia
- Frequency: 170/min.
- Identical and Wide QRS Complexes (> 0.12s)
- A re-entry impulse always exits in the same direction
- Therefore, all QRS complexes are identical
- P Waves are not visible
- They are hidden within the wide QRS complexes
- And the atria are activated retrogradely
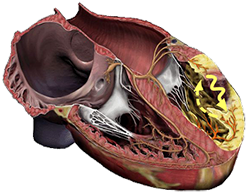
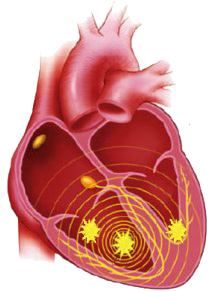
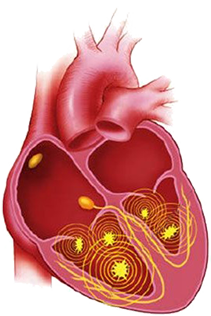
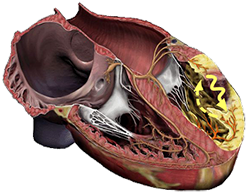
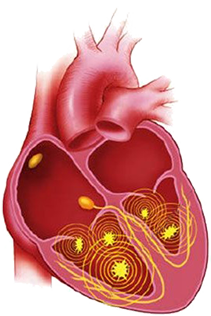
Polymorphic Ventricular Tachycardia
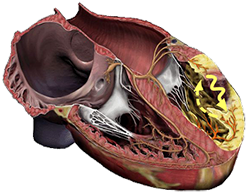
- Most commonly occurs during myocardial infarction
- Polymorphic VT more frequently progresses to ventricular fibrillation (compared to monomorphic VT)
- The mechanism is most often re-entry
- Torsades de Pointes
- QRS complexes are polymorphic (changing width and amplitude)
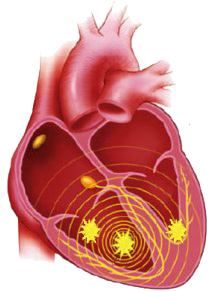
- In the ventricles, there are usually at least 3 ectopic foci
- Each activates the ventricles in a different direction (hence the change in shape of the QRS complexes)
- According to the number of foci in the ventricles, we recognize 3 mechanisms of polymorphic ventricular tachycardia
- Multifocal
- Bifocal
- Unifocal
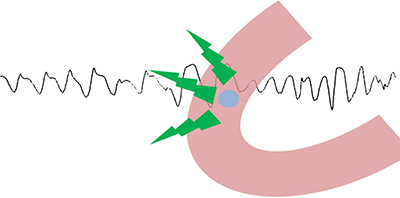
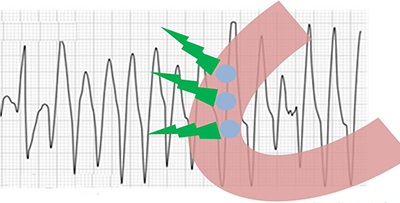
Multifocal Polymorphic VT
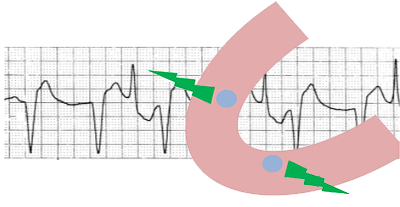
Bifocal Polymorphic VT
- There are 2 ectopic foci in the ventricles
- Vector from each focus has a different direction
- If the foci are opposite each other, the QRS axis changes by approximately 180°
- Occurs in bidirectional ventricular tachycardia
Unifocal Polymorphic VT
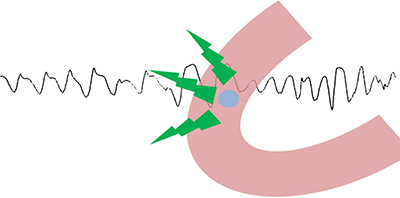
- There is 1 ectopic focus in the ventricles
- Vector from the focus changes direction
- Therefore, the QRS complexes are polymorphic
- Most commonly occurs in Torsades de Pointes (TdP)
Classification of Polymorphic Ventricular Tachycardia
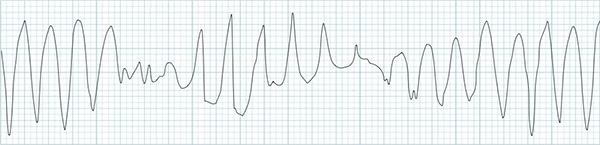
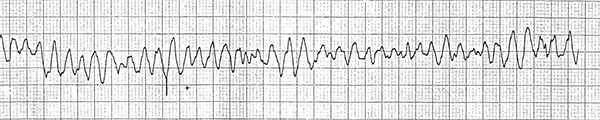
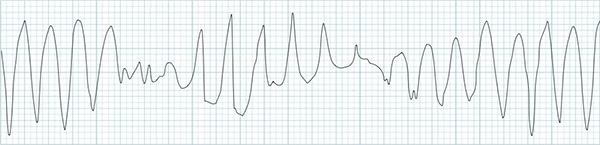
ECG and Polymorphic Ventricular Tachycardia
- Can have characteristic features of ventricular tachycardia
- Frequency 100-300/min.
- Wide QRS complexes (>0.12s)
- Width and amplitude vary (QRS complexes exhibit waviness)
- Can progress to ventricular fibrillation
- The key difference is that in ventricular fibrillation, the heart no longer functions as a pump
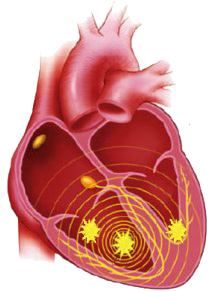
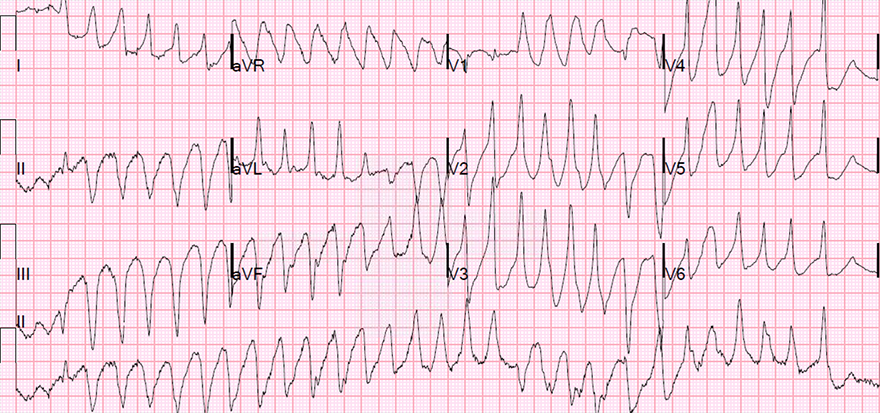
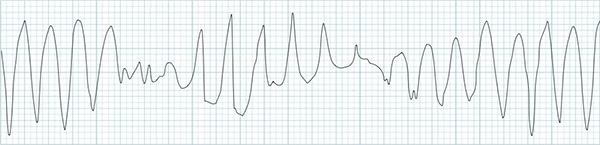
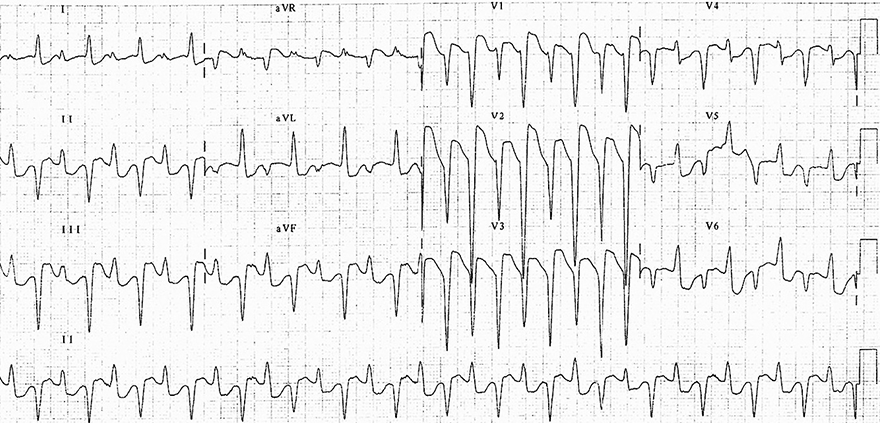
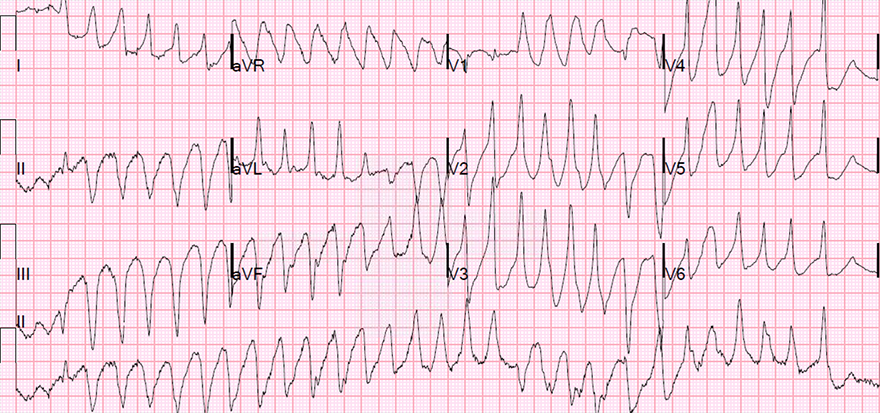
Polymorphic Ventricular Tachycardia
- In the ventricles, there are at least 3 ectopic foci (most commonly)
- Width and amplitude of QRS complexes change
- Features of ventricular tachycardia may be present
- The mechanism is most commonly triggered activity (Torsades de Pointes)
- Frequency is 100-300/min. (280/min. in this ECG)
- The heart still functions as a pump
- At frequencies > 160/min., it gradually stops functioning as a pump
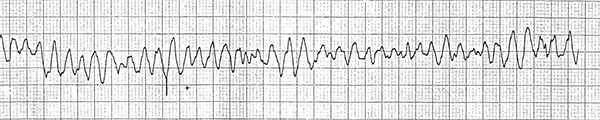
Polymorphic VT and Ventricular Fibrillation
- Polymorphic VT and ventricular fibrillation have a similar appearance on ECG
- Both have wide QRS complexes that change in width and amplitude
- ECG does not have precise criteria to differentiate between polymorphic VT and ventricular fibrillation
- The basic difference is that in ventricular fibrillation, the heart no longer functions as a pump
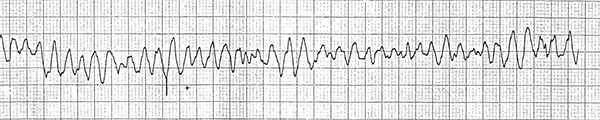
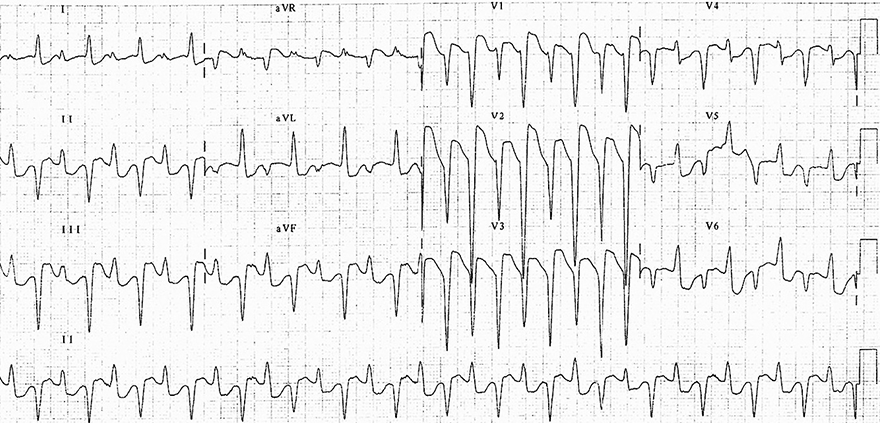
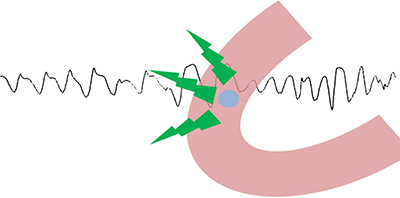
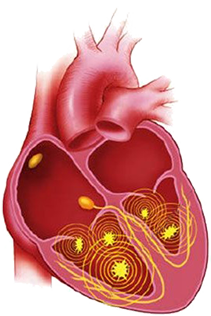
Ventricular Fibrillation
- In the ventricles, there are multiple foci
- The mechanism is most commonly micro re-entry
- Frequency is 300-450/min.
- Width and amplitude of QRS complexes change
- QRS complexes are low, and their amplitude is not precisely defined
- The heart does not function as a pump
- At such a high frequency, diastole is ineffective
- This is the basic difference from polymorphic VT
- Signs of ventricular tachycardia are not present
- QRS complexes decrease in amplitude and approximately 2 minutes later asystole occurs
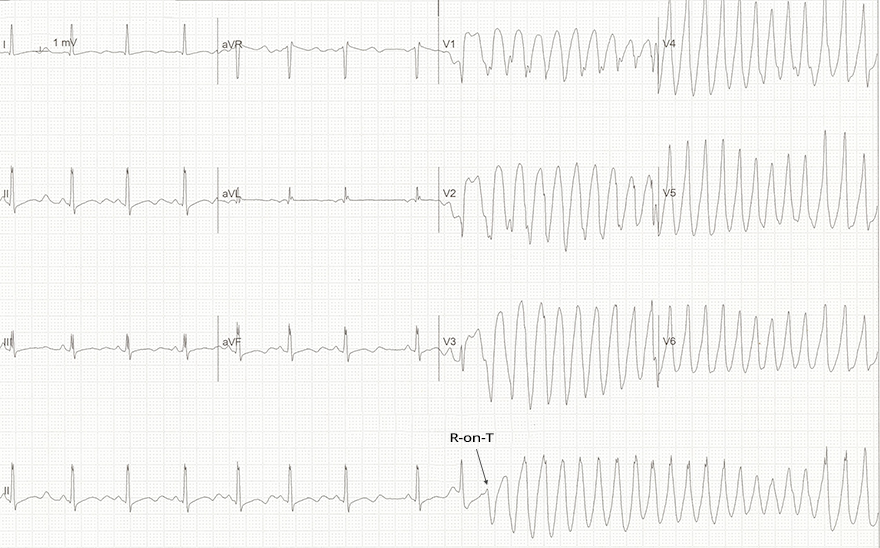
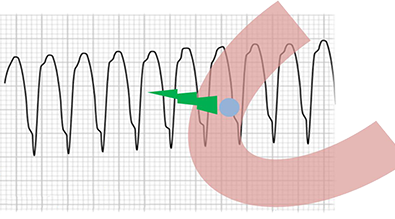
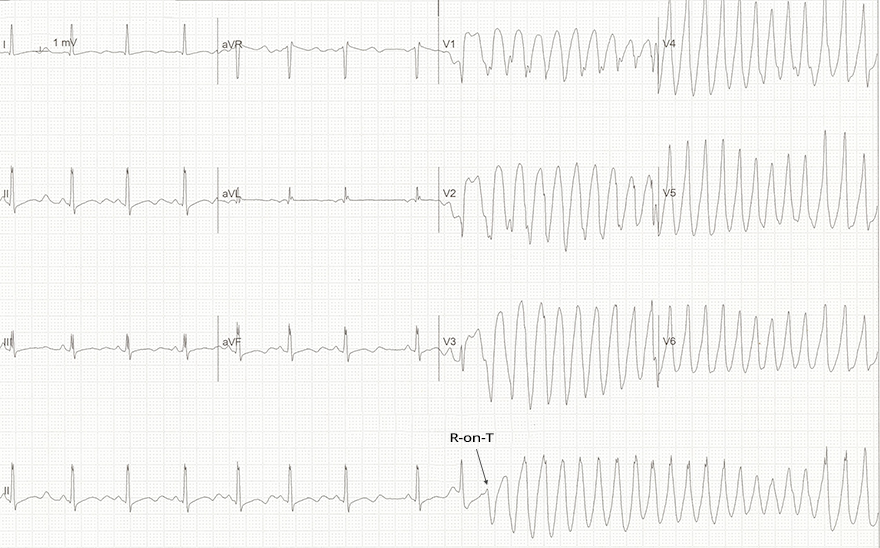
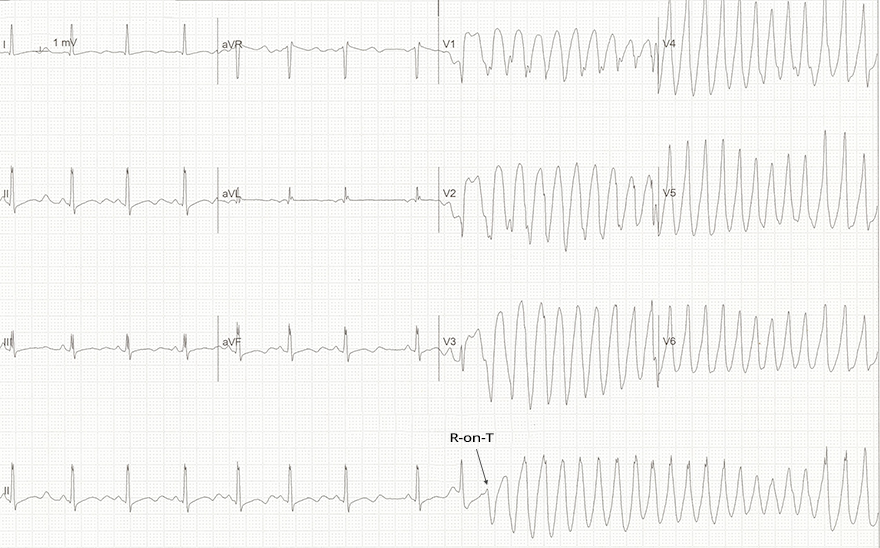
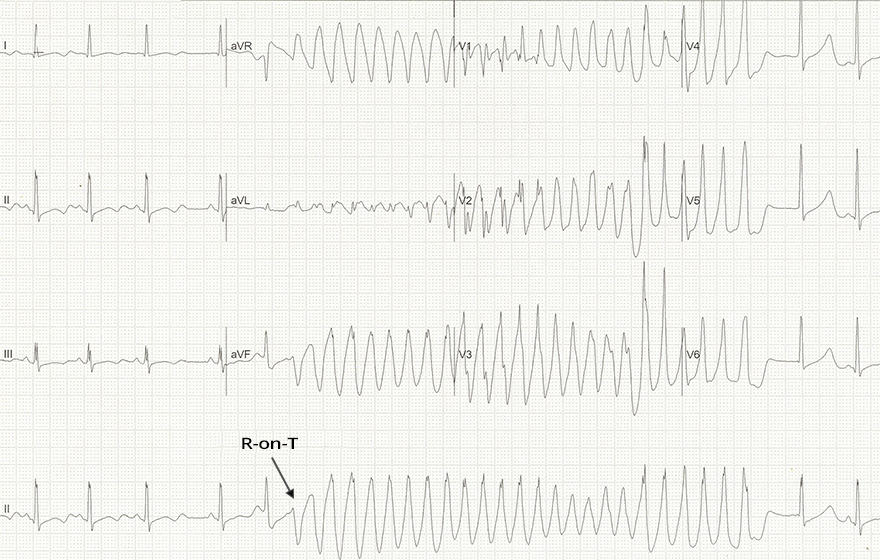
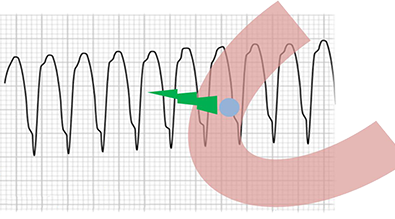
Polymorphic Ventricular Tachycardia (Torsades de Pointes)
Polymorphic Ventricular Tachycardia (Torsades de Pointes)
- Frequency 290/min.
- Wide QRS complexes that change in amplitude and width
- Again, the patient has severe hypokalemia (1.7 mmol/l)
- Ventricular extrasystole occurred on the T wave (R on T phenomenon)
- On the ECG is Torsades de Pointes
- Which is polymorphic VT that occurs with a prolonged QT interval
- In this case, there was spontaneous termination (resolution) of Torsades de Pointes after approximately 5 seconds
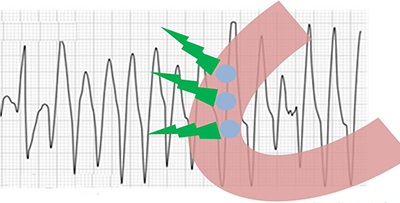
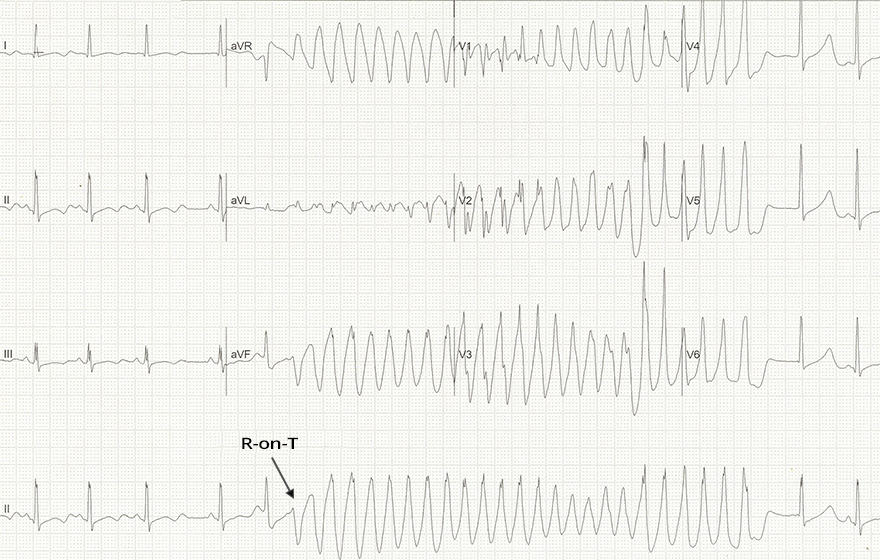
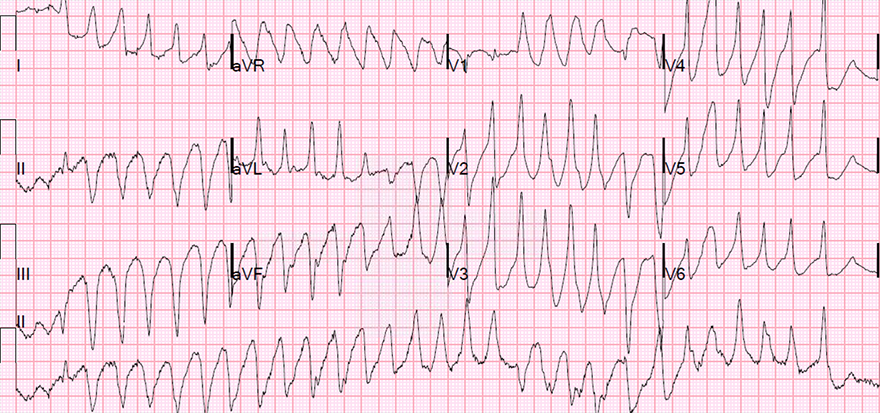
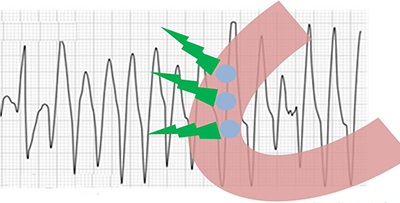
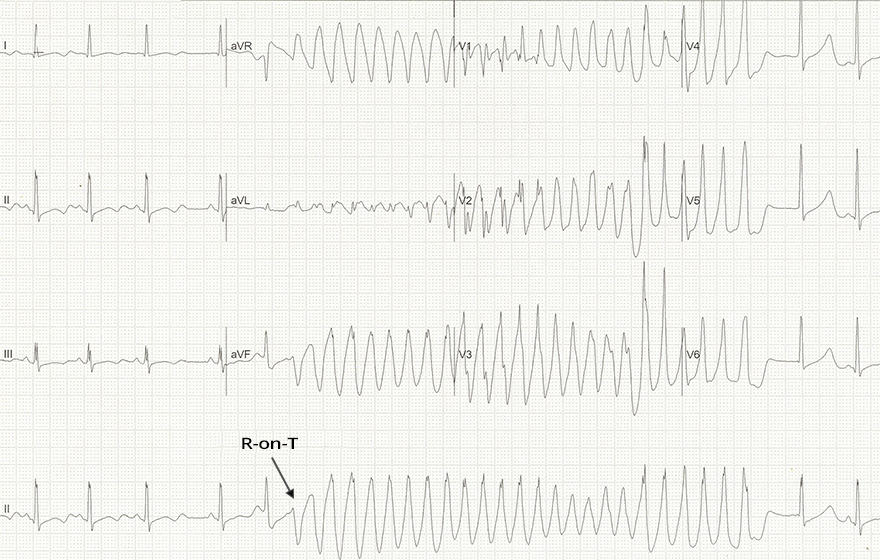
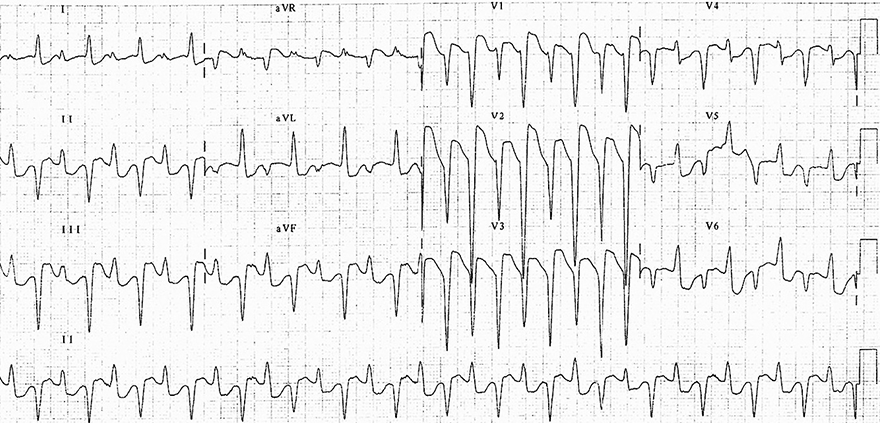
Polymorphic Ventricular Tachycardia
- Frequency: 200/min.
- QRS complexes are wide and vary in width and amplitude
- The patient had a previous ECG showing an inferior STEMI
- No prolonged QT interval was observed during sinus rhythm
- In this case, it is not Torsades de Pointes
- Polymorphic VT occurs during ischemia in the setting of an infarction
- In the continuous II lead (rhythm strip), we observe deformed QRS complexes with P waves (AV dissociation)

Polymorphic Ventricular Tachycardia (Torsades de Pointes) and Ventricular Fibrillation
Polymorphic Ventricular Tachycardia (Bidirectional Ventricular Tachycardia)
Sources
- ECG from Basics to Essentials Step by Step
- litfl.com
- ecgwaves.com
- metealpaslan.com
- medmastery.com
- uptodate.com
- ecgpedia.org
- wikipedia.org
- Strong Medicine
- Understanding Pacemakers