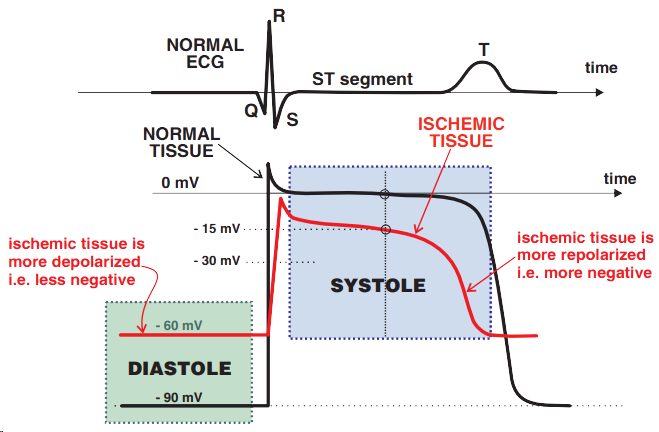
Ischemia During Diastole and Systole
Physiological ECG Recording
Subendocardial Ischemia


ST Depression and Ischemia
Flat Ascending ST Depression
Steep Ascending ST Depression
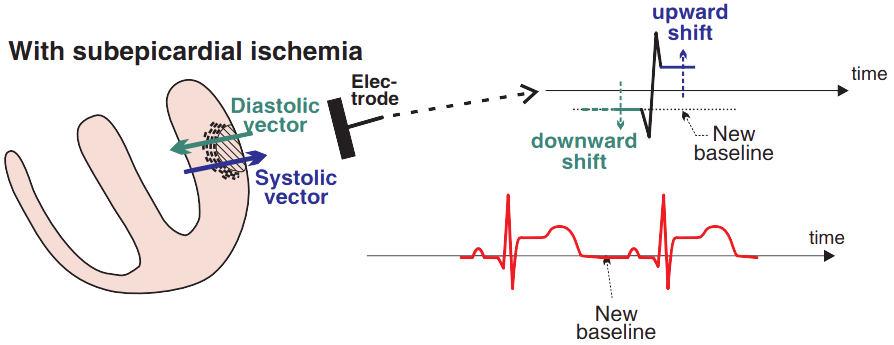
Subepicardial Ischemia
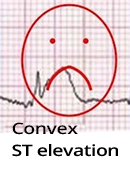
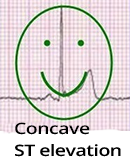

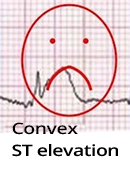
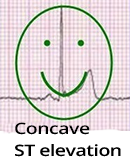
ST Elevations (STE) in Ischemia
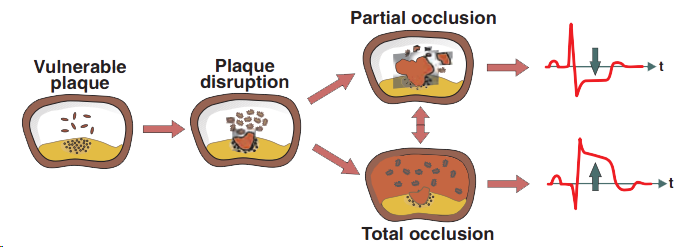
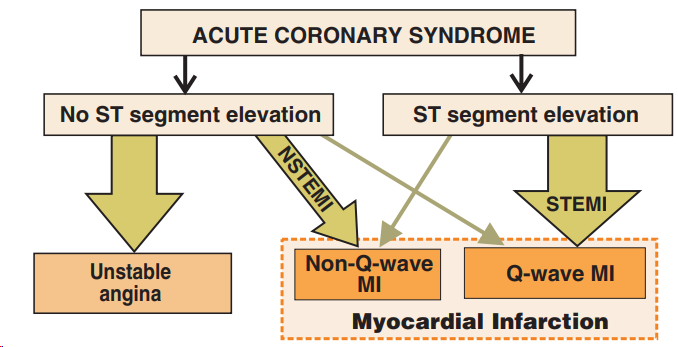
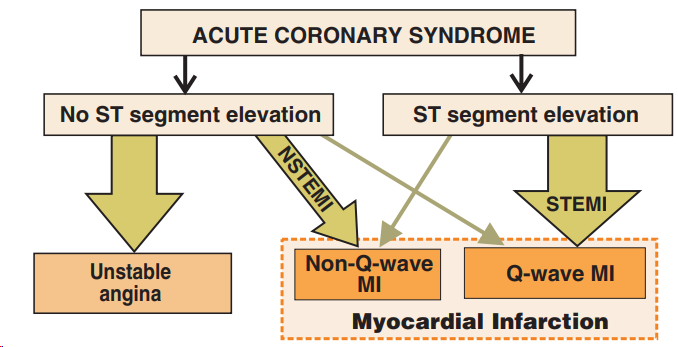
ST Segment and Acute Coronary Syndrome
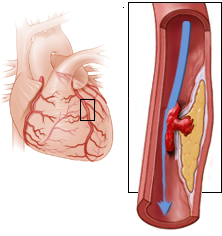

Unstable Angina Pectoris
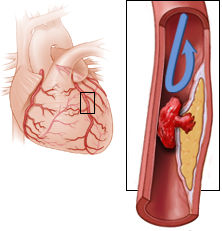
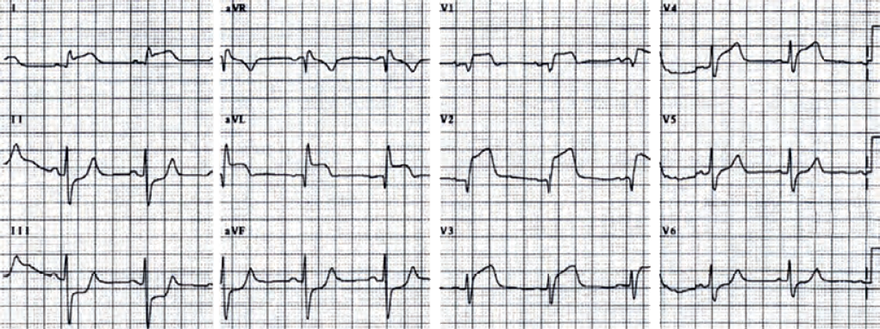
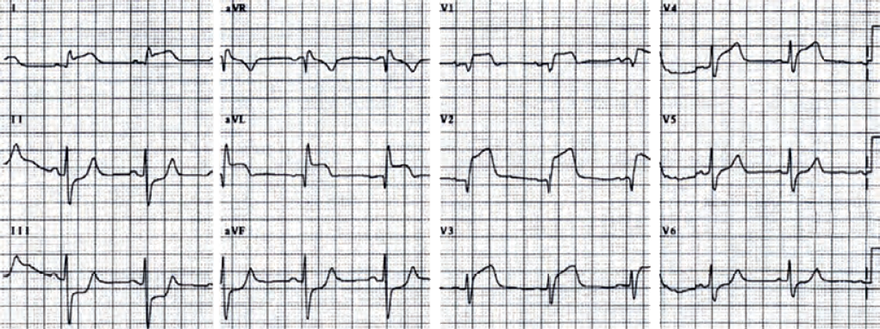
Acute STEMI of the Anterior Wall
Sources
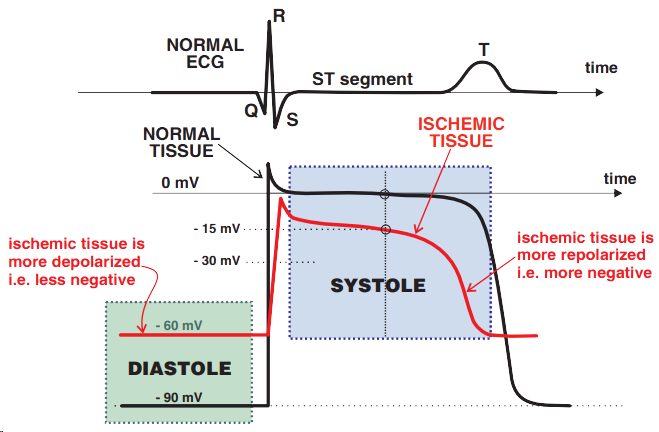
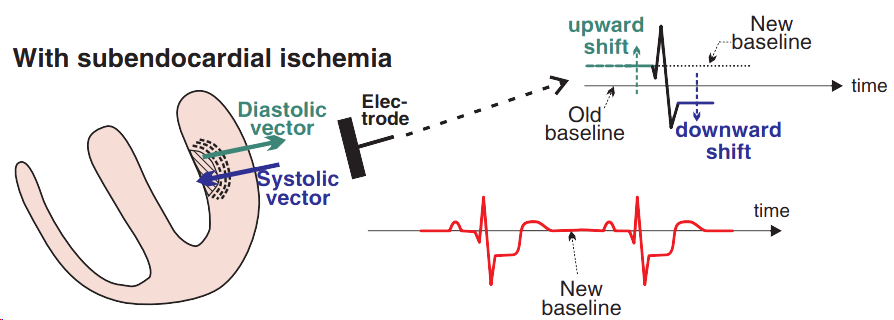
Ischemia During Diastole and Systole
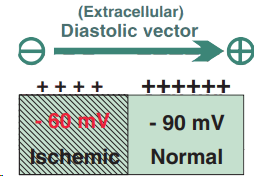
Ischemic Diastolic Vector
|
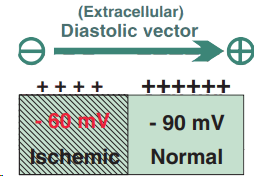
|
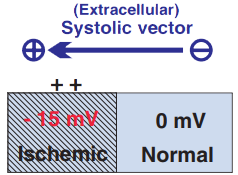
Ischemic Systolic Vector
|
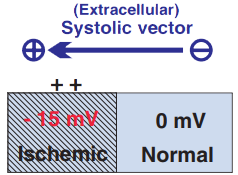
|
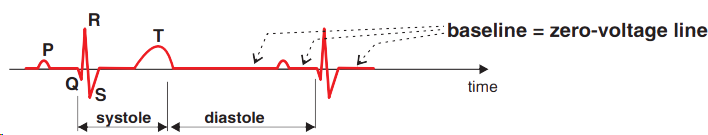
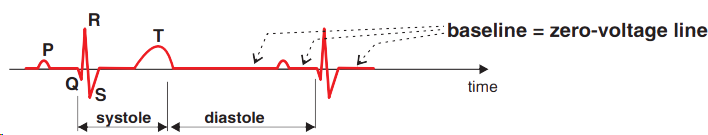
Physiological ECG Recording
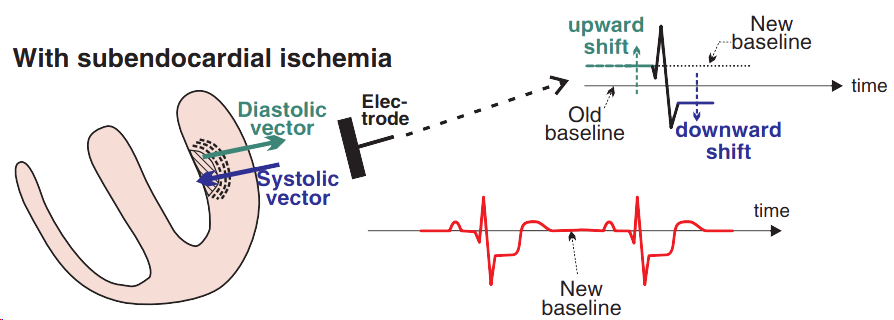
Subendocardial Ischemia

|

|
|
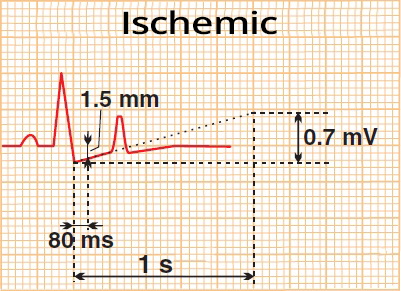
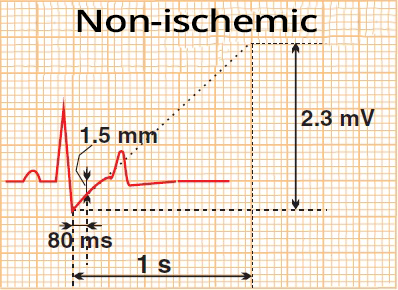
ST Depression and Ischemia
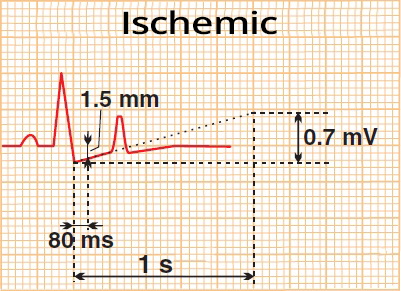
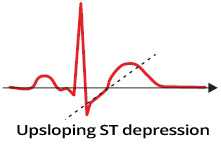
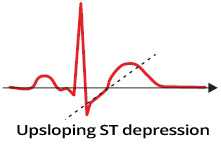
Flat Ascending ST Depression
|
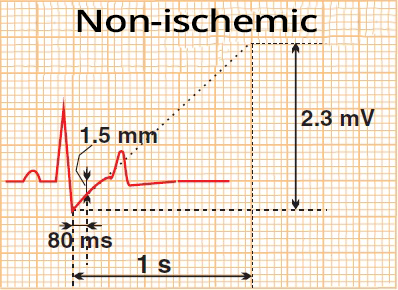
Steep Ascending ST Depression
|
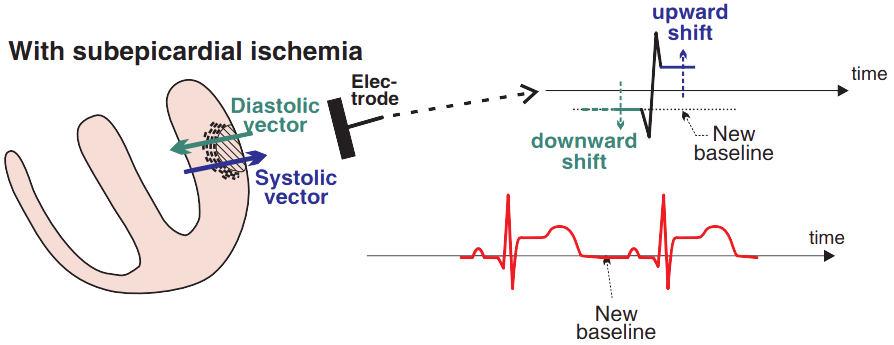
Subepicardial Ischemia
|
|

ST Elevations (STE) in Ischemia
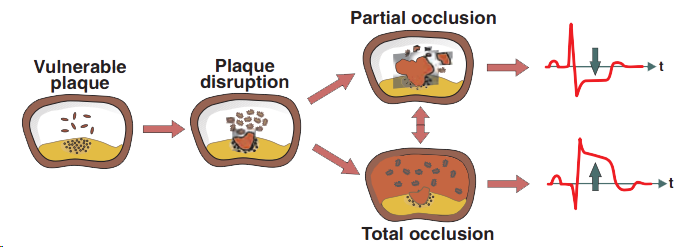
ST Segment and Acute Coronary Syndrome

|
Unstable Angina Pectoris
|
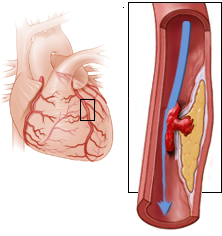
|
|
Acute STEMI of the Anterior Wall
|
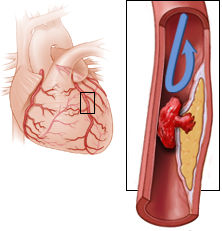
|
Sources