
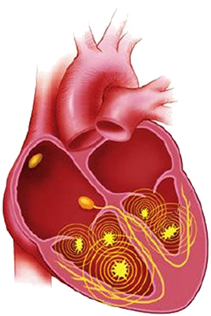
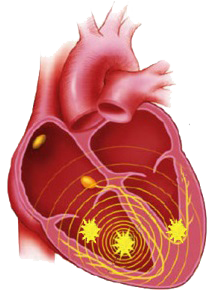
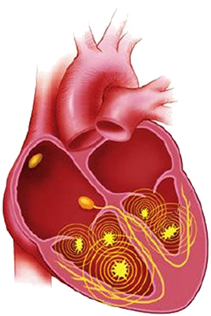
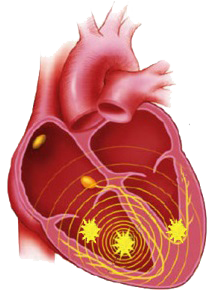
Multiple Micro Re-entries
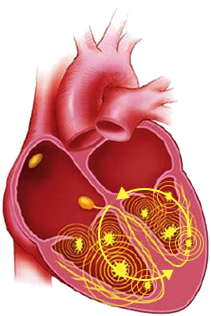
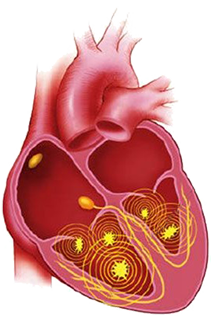
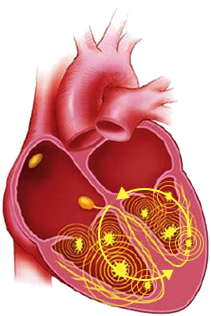
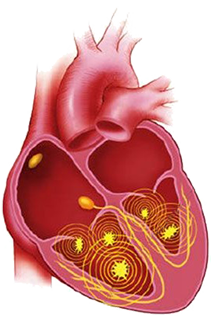
Mother Rotor Re-entry Circuit
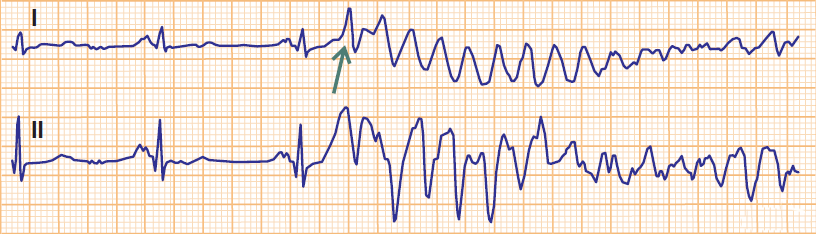
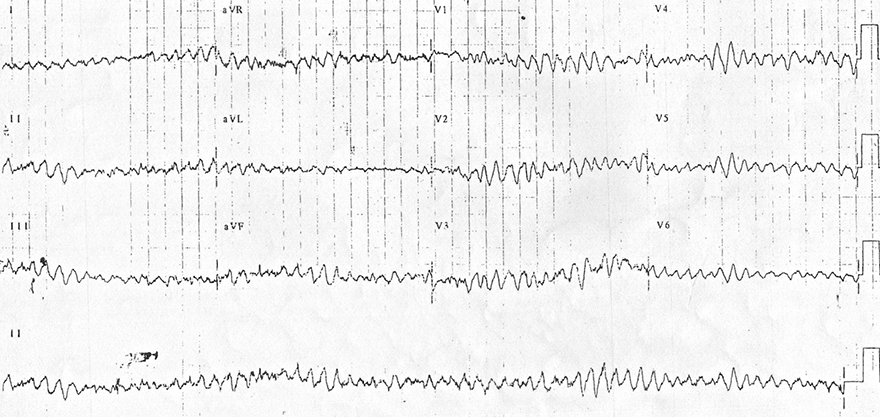
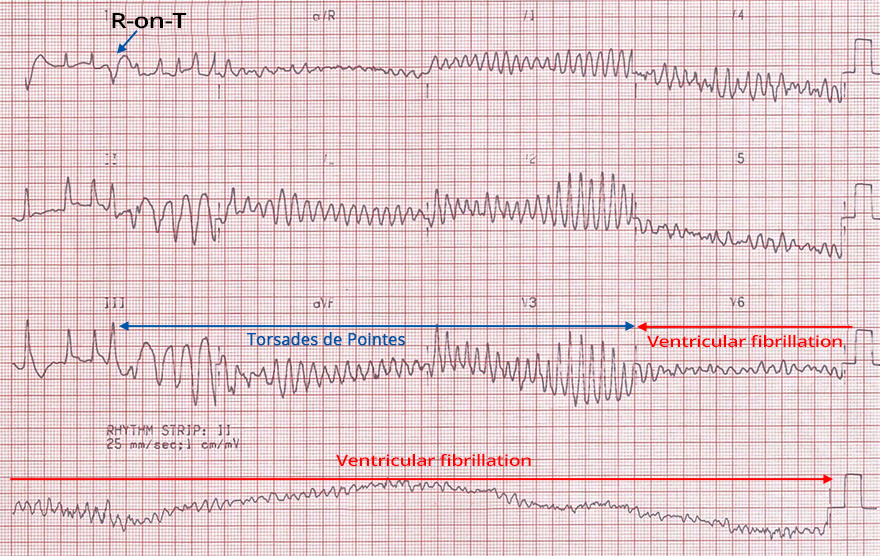
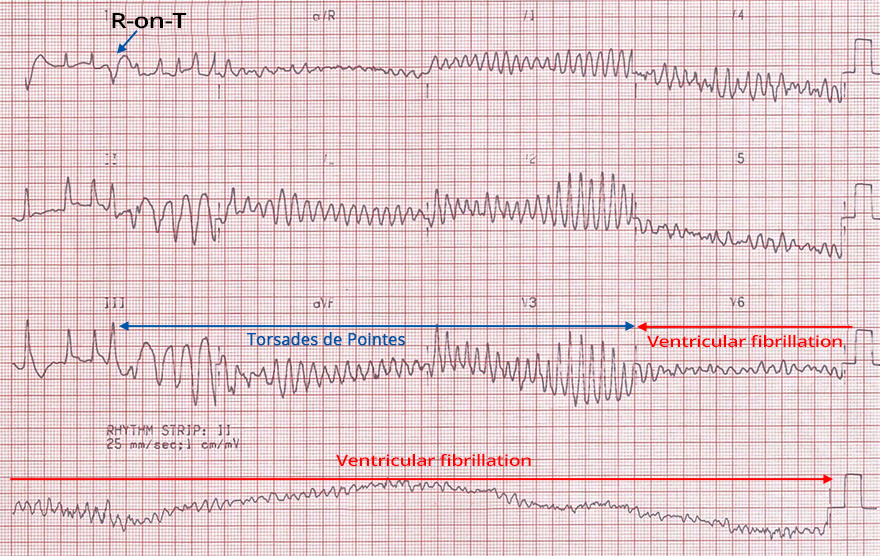
R-on-T Phenomenon and Ventricular Fibrillation
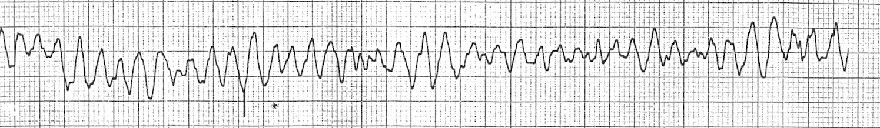
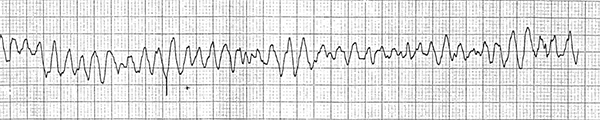
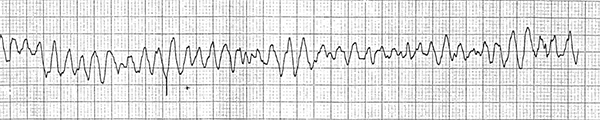
Coarse Ventricular Fibrillation

Fine Ventricular Fibrillation

Fine Ventricular Fibrillation and Asystole
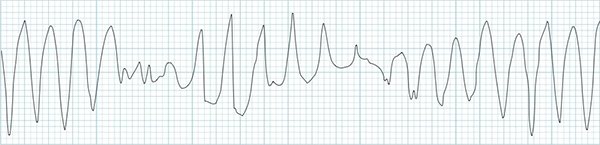
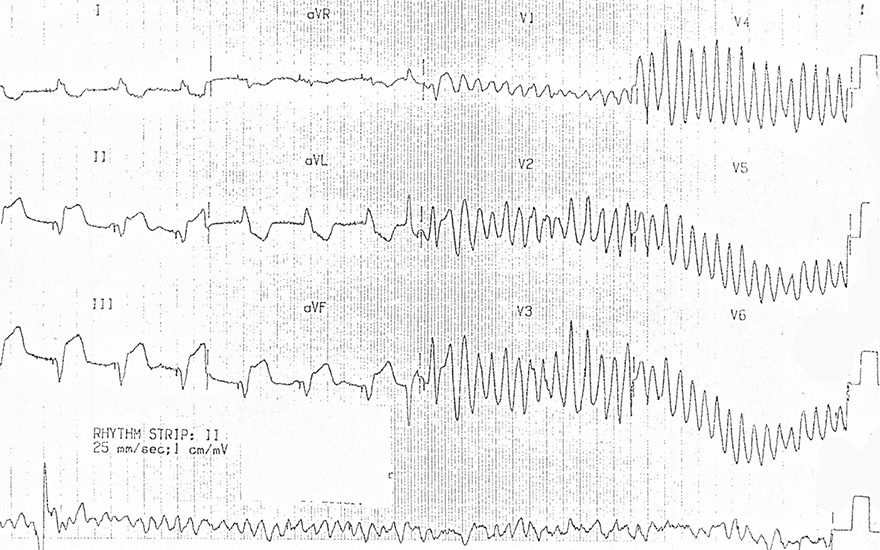
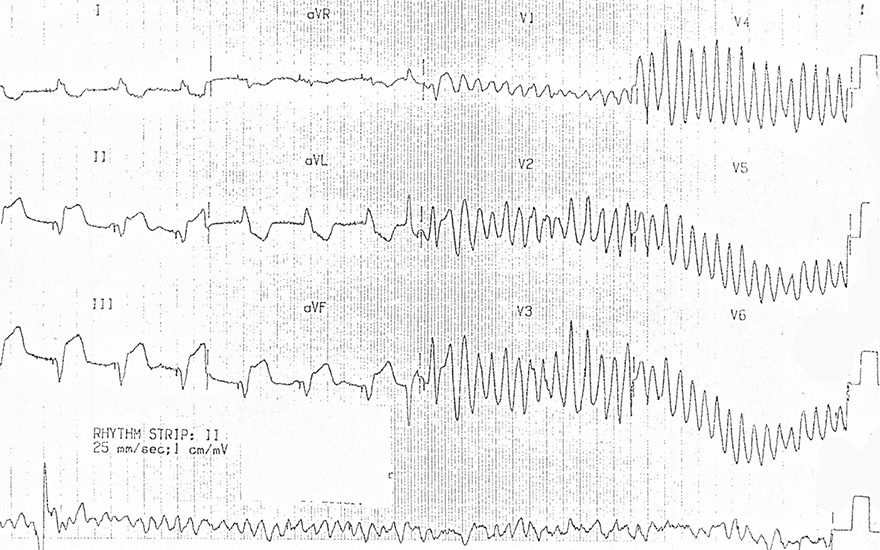
Polymorphic Ventricular Tachycardia
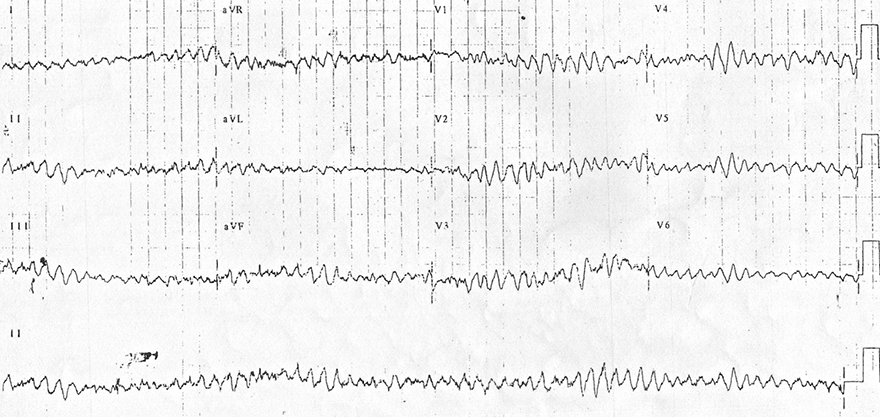
Ventricular Fibrillation





Ventricular Fibrillation

Ventricular Fibrillation

Ventricular Fibrillation

Ventricular Fibrillation and Accelerated Ventricular Rhythm
Sources
Ventricular Fibrillation
|

|
|
|
|
Multiple Micro Re-entries
|
Mother Rotor Re-entry Circuit
|
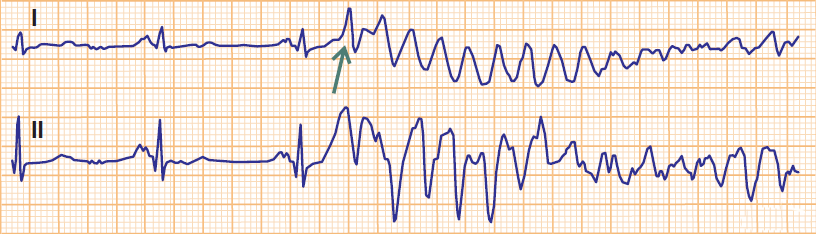
R-on-T Phenomenon and Ventricular Fibrillation
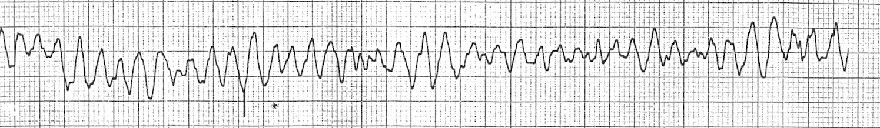
Coarse Ventricular Fibrillation

Fine Ventricular Fibrillation

Fine Ventricular Fibrillation and Asystole
|
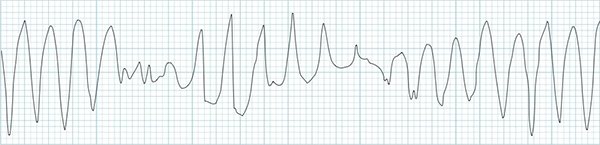
Polymorphic Ventricular Tachycardia
|
|
Ventricular Fibrillation
|
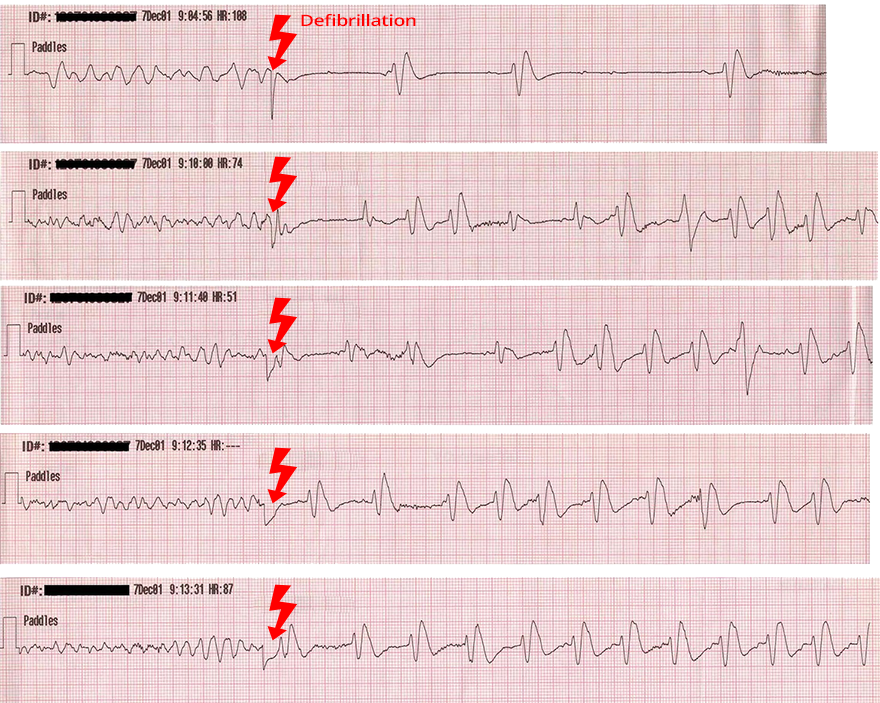
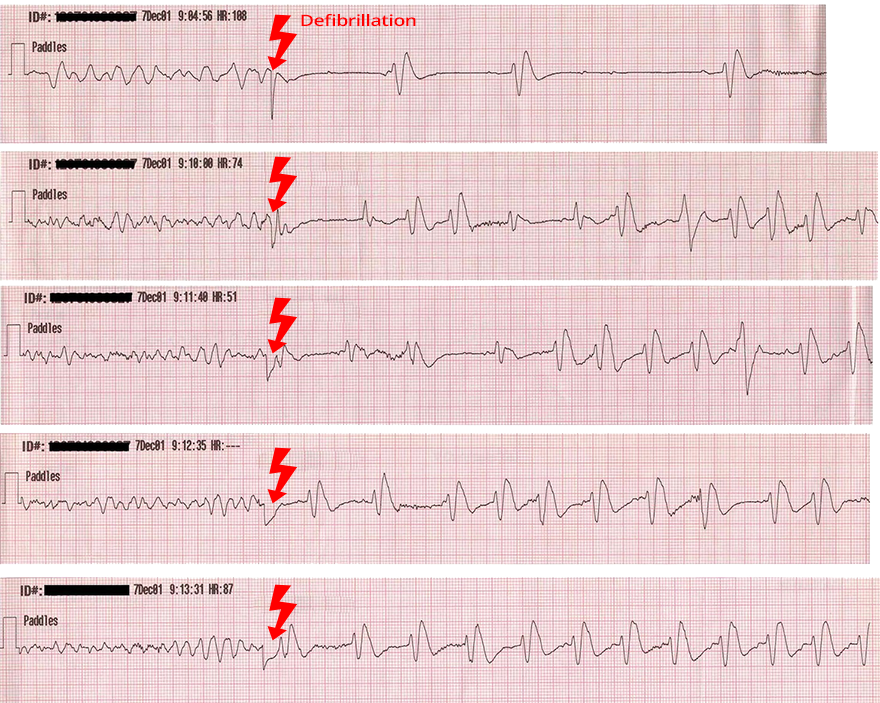
Defibrillator
|

|

|
 |
Defibrillation
|

|
|
Ventricular Fibrillation
|

|
|
Ventricular Fibrillation
|

|
|
Ventricular Fibrillation
|

|
|
Ventricular Fibrillation and Accelerated Ventricular Rhythm
|

|
Sources