Home /
Wolff-Parkinson-White (WPW) Syndrome - ECG
Pre-excitation syndrome, WPW syndrome, Atrioventricular bypass, Auriculoventricular accessory pathway syndrome
Preexcitation Syndrome

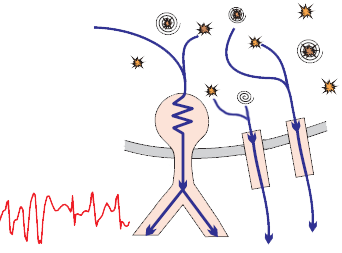
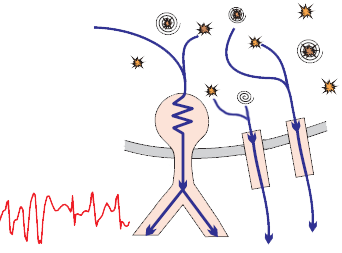
- Physiologically, the ventricles are activated through
- Preexcitation syndrome means
- that the ventricles are activated earlier
- The ventricles are pre-excited via an accessory pathway
- The most common accessory pathway is the Kent bundle
- Therefore, WPW syndrome is often referred to as
- Preexcitation syndrome (which is not entirely accurate)
- There are 3 preexcitation syndromes:
Wolff Parkinson White (WPW) Syndrome
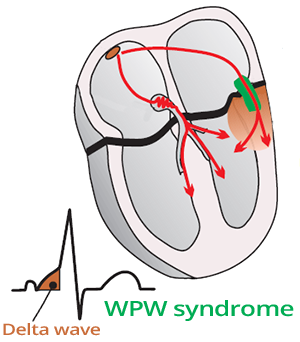
- WPW syndrome was described once in 1930 by cardiologists Wolff, Parkinson, and White
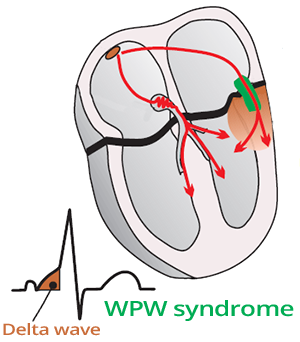
- Kent bundle
- It is an accessory connection in WPW syndrome, linking the atria and ventricles (Atrio-Ventricular bypass)
- About 0.5% of the population has it (it is a congenital anomaly)
- 10% of patients with Kent bundle also have an additional secondary accessory pathway
- Does not slow down impulse conduction like the AV node
- The impulse from the Kent bundle creates a Delta wave on the ECG
- Kent bundle (and any accessory pathway) can have
- Only Antegrade conduction (from atria to ventricles)
- Only Retrograde conduction (from ventricles to atria)
- Or conduction in both directions
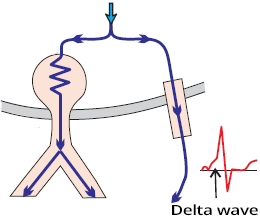
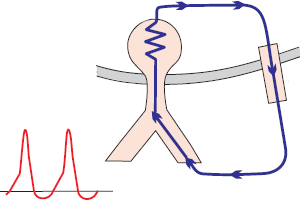
Delta Wave and WPW Syndrome
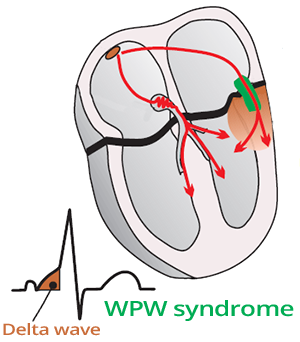
- Kent bundle activates one ventricle earlier than the impulse from the AV junction
- The impulse from the Kent bundle creates a delta wave on the ECG
- Delta wave
- Fusion beat (fusion beat)
ECG and WPW Syndrome
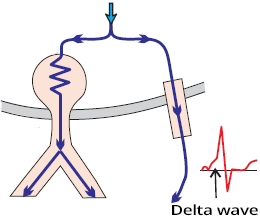
- Shortened PQ interval < 0.12s
- Delta wave (Arises due to early activation of part of the ventricle via the Kent bundle)
- Widened QRS complex > 0.11s (QRS complex is widened due to the delta wave)
- Pathological Q wave in the inferior leads (II, III, aVF)
- High R wave in the precordial leads
- ECG signs of WPW syndrome are present
- Only if the anterograde conduction through the Kent bundle is faster than conduction through the AV junction

WPW Syndrome
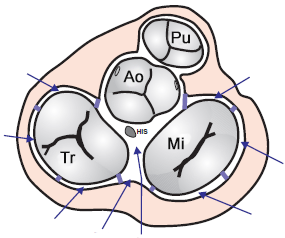
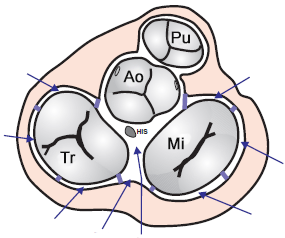
Localization of Kent's Bundle
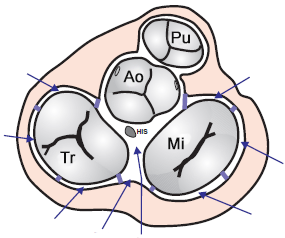
- Kent's bundle is most commonly found in:
- Left atrium: 46-60%
- Right atrium: 13-21%
- Postero-septal: 25%
- Anterior-septal: 2%
- d'Avila algorithm
- Can localize Kent's bundle with 90% accuracy
- Into 8 anatomical sites
- For localizing Kent's bundle in the left and right atrium
- Leads V1 and V6 are used
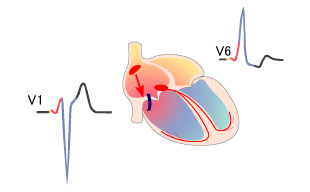
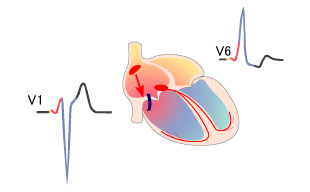
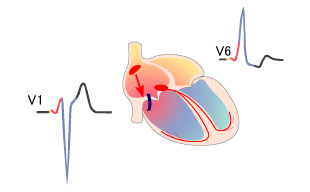
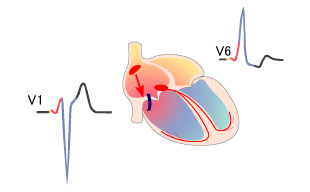
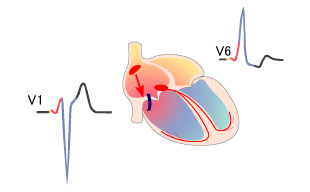
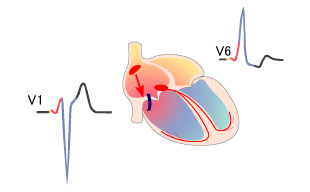
- WPW syndrome type A (left atrium)
- Kent's bundle connects the left atrium - left ventricle
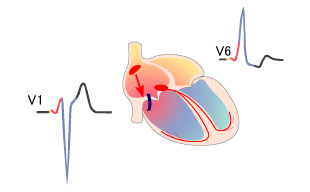
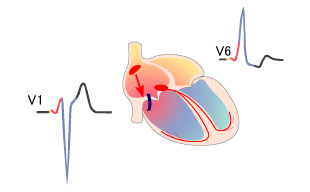
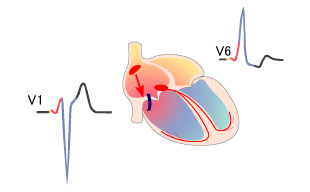
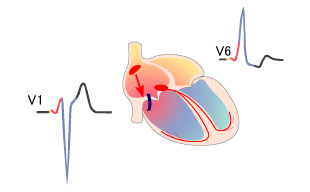
- WPW syndrome type B (right atrium)
- Kent's bundle connects the right atrium - right ventricle
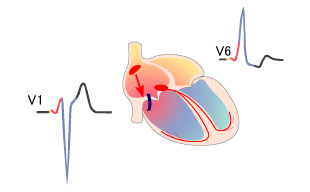
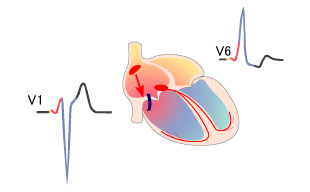
WPW Syndrome Type A (Left Atrial Pathway)

- Kent's bundle connects the left atrium + left ventricle
- The impulse pre-excites the left ventricle, then spreads throughout the myocardium
- The QRS resembles a Right Bundle Branch Block
- QRS complex is positive in V1
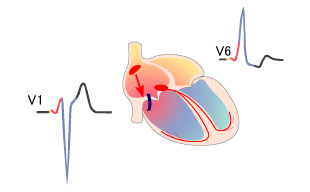
WPW Syndrome Type B (Right Atrial Pathway)
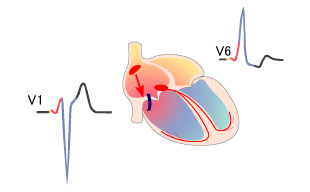
- The Kent bundle connects the right atrium + right ventricle
- The impulse pre-excites the right ventricle, then spreads to the entire myocardium
- The QRS complex resembles Left Bundle Branch Block
- The QRS complex is negative in V1
Differential Diagnosis of WPW Syndrome
Manifest Kent Bundle
- Anterograde conduction through the Kent bundle is faster than conduction through the AV node
- 25% of patients with anterograde conduction have blocked retrograde conduction
- Antidromic AVRT may occur
- Orthodromic AVRT cannot occur
- 10% of patients with the Kent bundle have an additional secondary accessory pathway
- Degree of preexcitation
- The wider the QRS complex (Delta wave), the larger part of the ventricles is pre-excited
- Preexcitation (QRS width) depends on heart rate
- With increasing heart rate, conduction through the AV junction speeds up and the QRS complex narrows
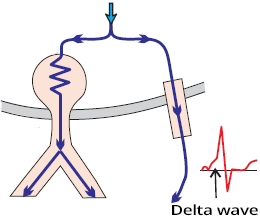
ECG (Delta Wave)
- The ECG shows a Delta wave
- Because the impulse through the Kent bundle begins to activate the ventricles earlier
- Than the impulse through the AV junction
Latent Kent Bundle
- The Kent bundle has anterograde conduction
- The ventricles are activated simultaneously via the AV junction and the Kent bundle
- No Delta wave on the ECG
- It is obscured by the QRS complex
- The ECG shows a sinus rhythm with a narrow QRS complex
- The Kent bundle is latent if it is lateral in the left atrium
- Because the impulse from the SA node has to travel a long path to the Kent bundle
- The latent Kent bundle is unmasked by atrial pacing in the left atrium (Delta wave appears on the ECG)
ECG (Narrow QRS without Delta Wave)
- The ECG shows a narrow QRS complex without a Delta wave
- The ventricles are activated simultaneously via the AV junction and the Kent bundle
- The Delta wave is obscured by the narrow QRS complex
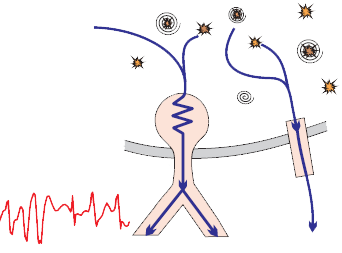
Concealed Conduction through the Kent Bundle
- The Kent bundle can conduct impulses both anterogradely and retrogradely, but they are blocked
- This is concealed conduction (Concealed conduction), because it is not visible on the ECG under normal circumstances
- Retrograde conduction is unmasked during orthodromic AVRT
- Antegrade conduction is unmasked during atrial fibrillation
- Benign Accessory Pathway
- The Kent bundle with a long refractory period is referred to as a benign accessory pathway
- Because during supraventricular tachycardia (most commonly atrial fibrillation), it acts as a filter for impulses
ECG (Narrow QRS without Delta Wave)
- The ECG shows a narrow QRS complex without a Delta wave
- Because the ventricles are activated only through the AV junction
- The impulse through the Kent bundle is blocked, and the Delta wave does not appear
- The ECG appearance is the same as with a latent Kent bundle
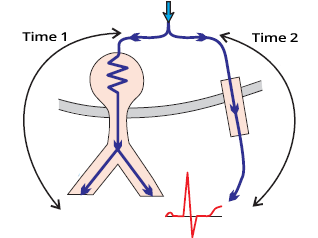
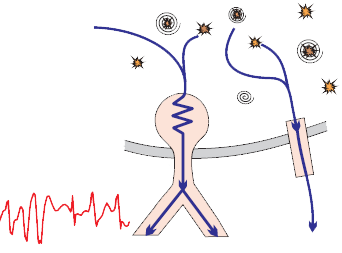
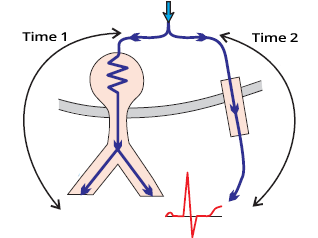
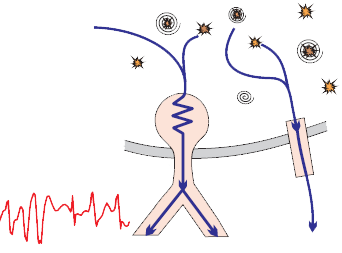
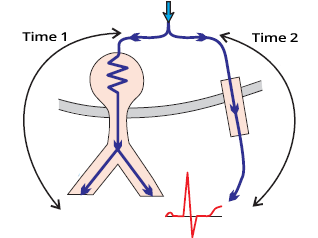
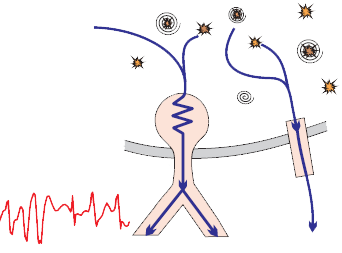
Orthodromic AVRT
- Atrioventricular reentry tachycardia (AVRT) has a macro re-entry circuit between the atria and ventricles
- The impulse circulating in the re-entry circuit can trigger ventricular or atrial extrasystoles
- Based on the direction of the impulse, we distinguish 2 types of AVRT:
- Antidromic AVRT (5% of all AVRT)
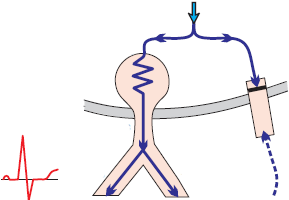
- Orthodromic AVRT (95% of all AVRT), where the impulse circulates:
- Anterogradely through the AV junction as in sinus rhythm, hence the QRS complexes are narrow
- Retrogradely through the Kent bundle, with the atria activated through the Kent bundle
- P waves are after the QRS complex (often hidden in the T wave)

ECG (Narrow QRS)
- Orthodromic AVRT
- Narrow QRS complexes, without a Delta wave
- The ventricles are activated through the AV junction
- The atria are activated through the Kent bundle
- P waves are after the QRS complex (often hidden in the T wave)
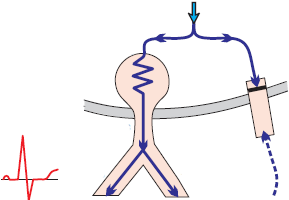
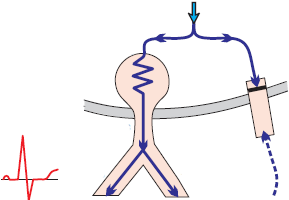
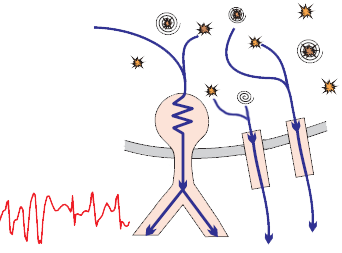
Antidromic AVRT
- Antidromic AVRT (5% of all AVRT)
- The circulating impulse in the re-entry circuit can trigger ventricular or atrial extrasystoles
- The impulse circulates:
- Anterogradely through the Kent bundle
- The ventricles are activated through the Kent bundle, resulting in wide QRS complexes (Delta wave is present)
- Retrogradely through the AV junction
- The atria are activated through the AV junction. P waves are before the QRS complex (often hidden in the T wave)
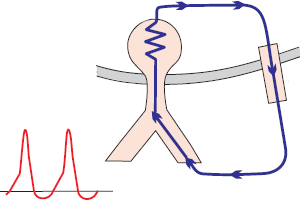
ECG (Wide QRS and Delta wave)
- Antidromic AVRT
- Wide QRS complexes, with Delta wave
- The ventricles are activated through the Kent bundle
- The atria are activated through the AV junction
- P waves are before the QRS complex (often hidden in the T wave)
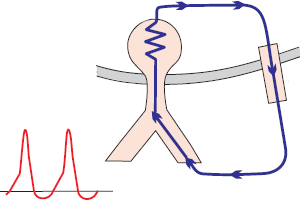
Atrial Fibrillation and WPW Syndrome
- 20% of patients with WPW syndrome have Atrial Fibrillation
- In Atrial Fibrillation, there are numerous micro re-entry circuits in the atria
- which generate impulses irregularly at a rate of 350-600/min.
- The Kent bundle does not filter impulses from the atria like the AV junction
- The ventricles are primarily irregularly activated through the Kent bundle (Wide QRS complexes)
- Intermittently, they are also irregularly activated through the AV junction (Narrow QRS complexes)
- Can result in
- Fusion beat (Fusion contraction) where the ventricles are activated simultaneously through the AV junction and Kent bundle
- Capture beat (Captured contraction) where the ventricles are activated only through the AV junction
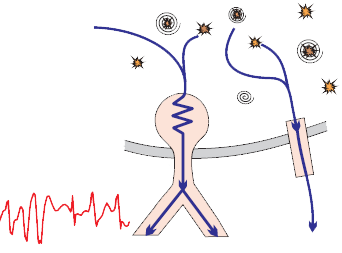
ECG (Wide QRS and Delta wave)
- Atrial Fibrillation with WPW syndrome
- The ventricles are primarily activated through the accessory pathway
- Wide QRS complexes occur (due to the Delta wave)
- Can reach a rate of up to 200-300/min.
- If impulses intermittently pass through the AV junction, it can result in
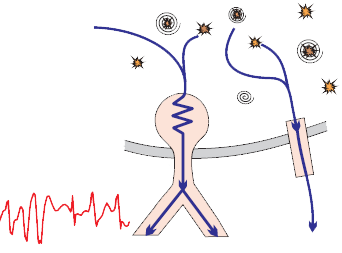
Malignant Accessory Pathway

- Has a short refractory period, allowing it to conduct impulses at high frequencies
- Malignant accessory pathway in supraventricular tachycardia
- Conducts impulses to the ventricles at a rate of 200-300/min.
- Progressively leads to ventricular fibrillation and the heart stops functioning as a pump
- A patient with WPW syndrome is at risk from any supraventricular tachycardia, most commonly
Benign Accessory Pathway
- Has a long refractory period, so it cannot conduct impulses to the ventricles at high frequencies
- This pathway is inactive during sinus rhythm
- It is a concealed conduction because the accessory pathway blocks the second impulse during the refractory period and resets
- No signs of pre-excitation are present on the ECG
- The accessory pathway becomes evident during tachycardia
- During sinus rhythm, delta waves may intermittently appear (if it is WPW syndrome)
- When a supraventricular impulse passes to the ventricles through the accessory pathway outside the refractory period

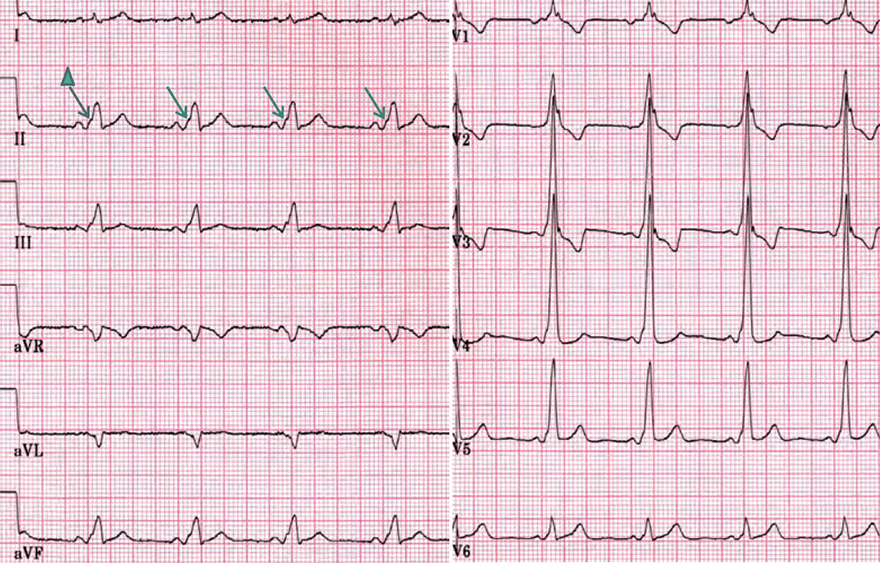
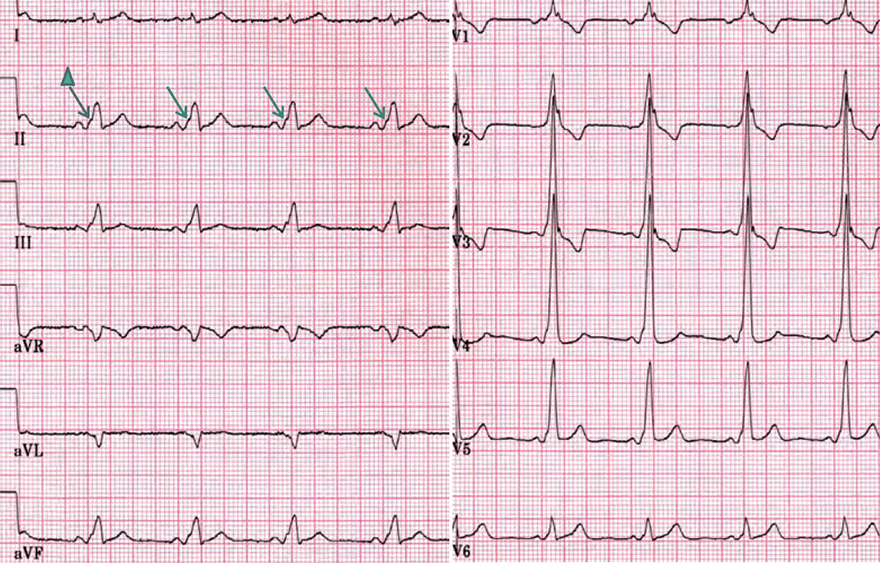
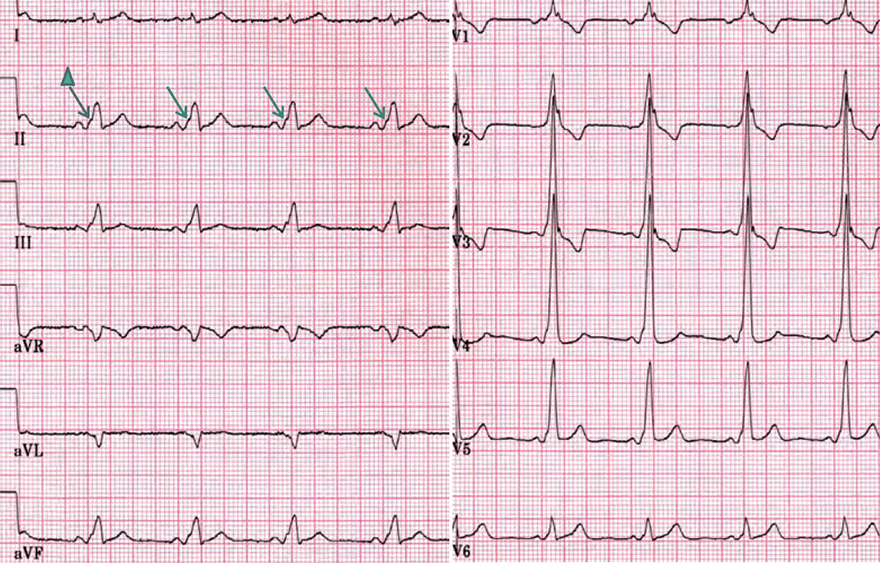
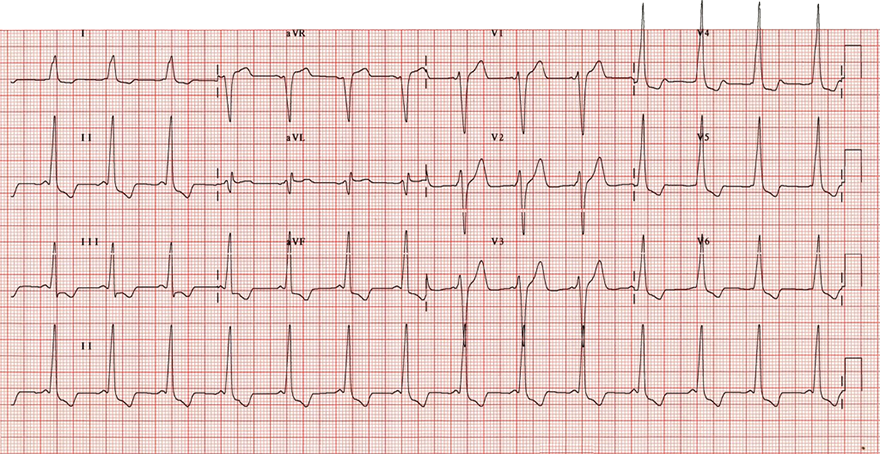
WPW Syndrome (Type A)


WPW Syndrome (Type A)
- Shortened PQ interval < 0.12s
- Delta wave and wide QRS approximately 0.15s
- Dominant QRS and Delta wave (V1)
- This indicates that the Kent bundle is in the left atrium
- Dominant R wave in V1-V3
- Pathological Q (aVL)

WPW Syndrome (Type A)
- Shortened PQ interval < 0.12s
- Delta wave and widened QRS about 0.15s
- Dominant QRS and Delta wave (V1)
- This indicates that the Kent bundle is in the left atrium
- Dominant R wave in V1-V3
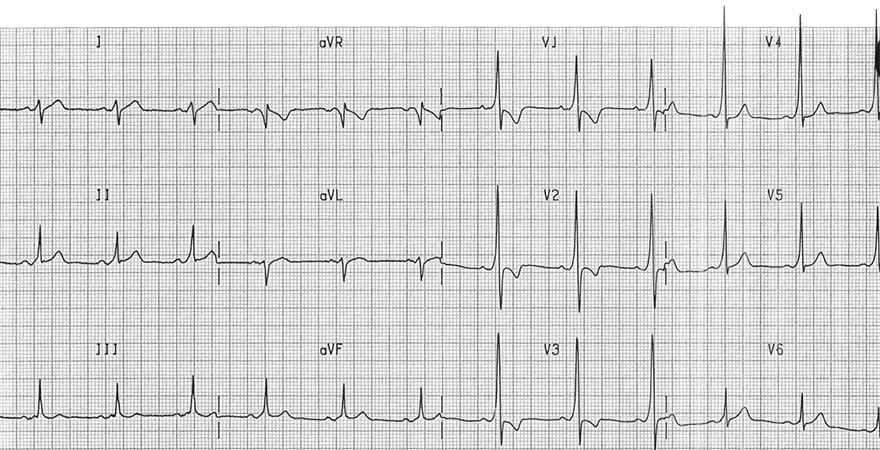
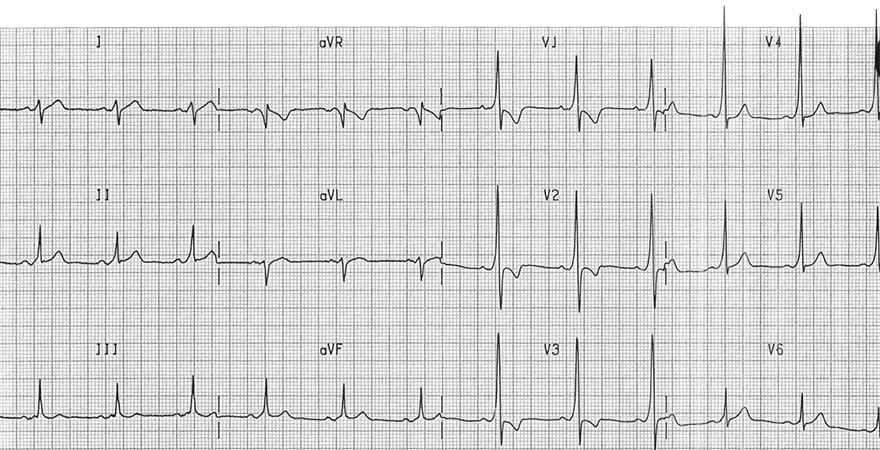
WPW Syndrome (Type B)
- Shortened PQ interval < 0.12s
- Delta wave and widened QRS about 0.15s
- Negative QRS (V1)
- This indicates that the Kent bundle is in the right atrium
- Dominant R wave in V4-V6, not due to:

WPW Syndrome (Type B)
- Shortened PQ interval < 0.12s
- Delta wave and widened QRS about 0.15s
- Negative QRS (V1)
- This indicates that the Kent bundle is in the right atrium
- Dominant R wave in V4-V6, not due to:
- Pathological Q wave (III and aVF)

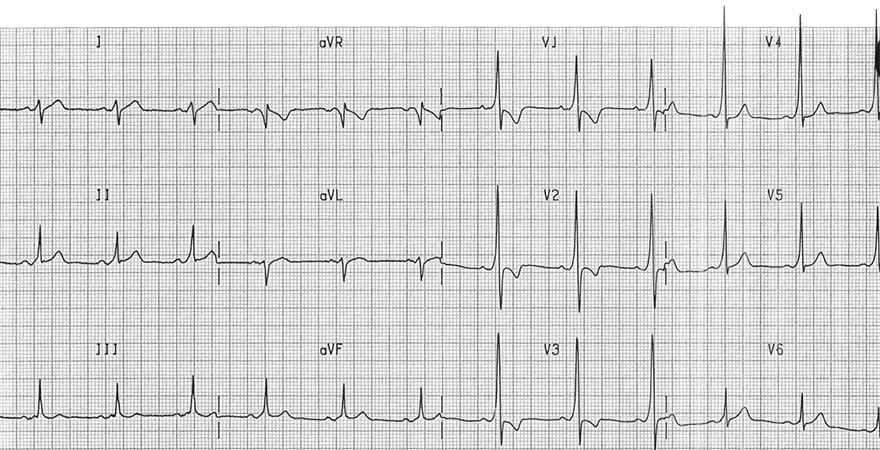
Intermittent WPW Syndrome (Type B)
- The ECG shows sinus rhythm
- During sinus rhythm, the Kent bundle blocks impulses
- Impulses pass to the ventricles only through the AV junction
- Intermittently, widened QRS complexes with delta wave appear
- The Kent bundle is in the right atrium
- Widened QRS complexes with Delta wave are negative in V1 lead

Intermittent WPW Syndrome (Type B)
- On the ECG, there is a alternation between WPW syndrome and sinus rhythm
- Mainly, we see widened QRS complexes with delta wave (WPW syndrome)
- The Kent bundle is in the right atrium
- Widened QRS complexes with Delta wave are negative in the V1 lead

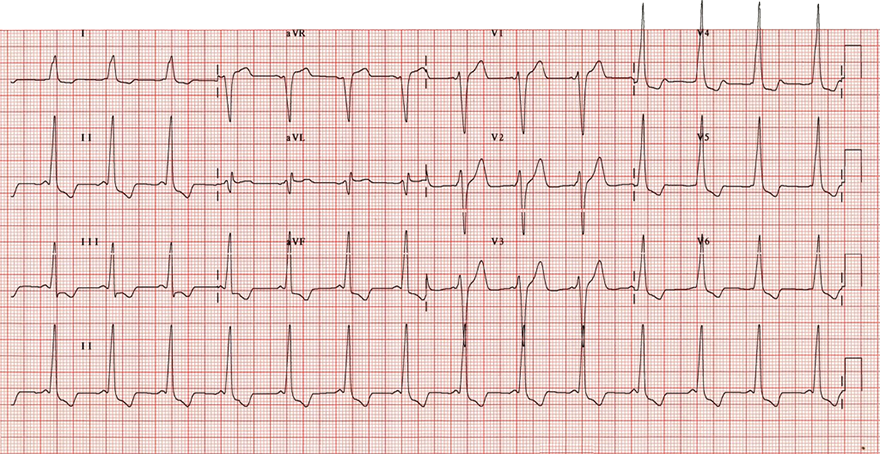
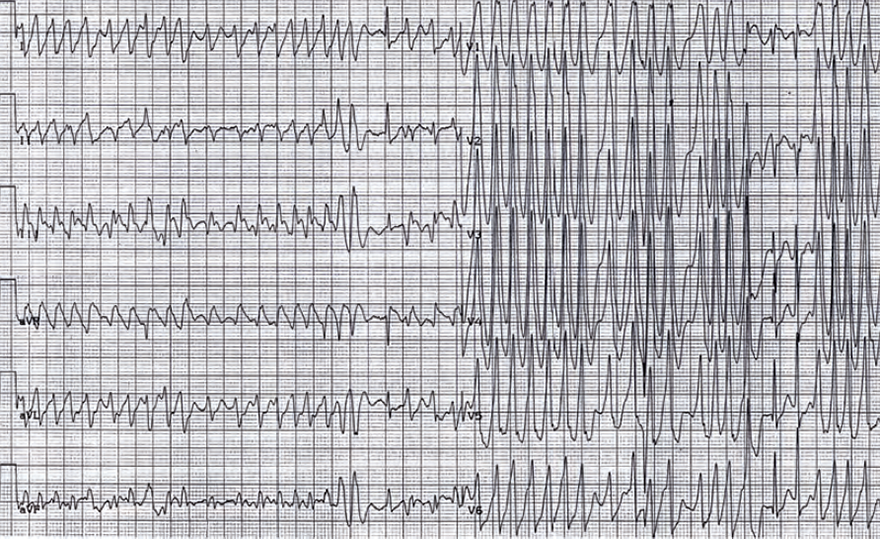
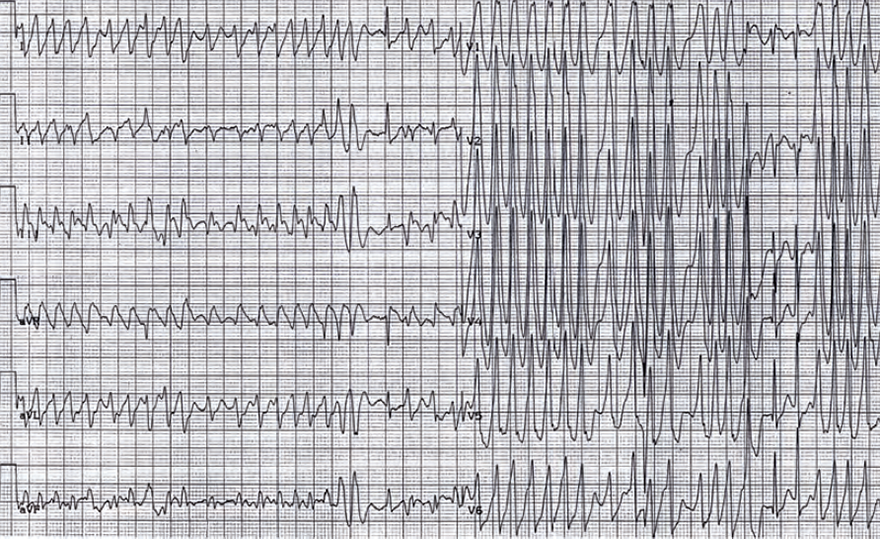
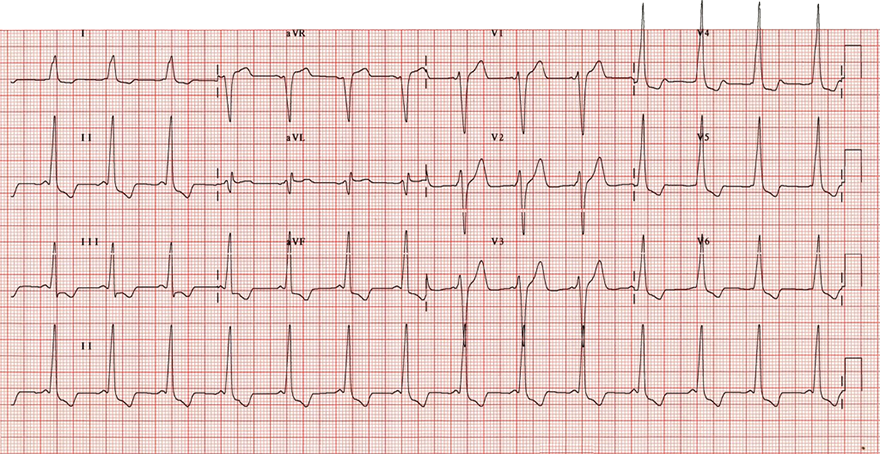
WPW Syndrome and Atrial Fibrillation
- Widened QRS complexes with Delta wave
- The heart rate is irregular with a frequency of 300/min.
- The patient has atrial fibrillation
- Impulses pass to the ventricles through the Kent bundle
- The patient has a malignant accessory pathway
- Because the pathway conducted impulses at 300/min.
- Ventricular fibrillation quickly develops
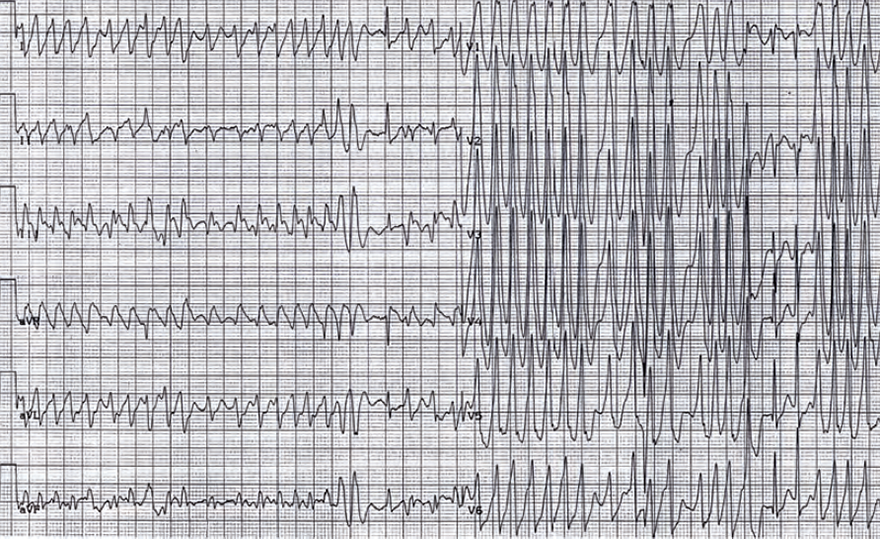
WPW Syndrome and Atrial Fibrillation
- Widened QRS complexes with Delta wave
- The heart rate is irregular with a frequency of approximately 300/min.
- The morphology of the QRS complexes changes
- In the center of the ECG, a capture beat appears to be present
- The ventricles were activated only through the AV junction
- We see 2 different QRS complexes with Delta wave (lead II)
- The patient has 2 accessory pathways (2 Kent bundles)
- Through which impulses alternately pass to the ventricles
Sources
- ECG from Basics to Essentials Step by Step
- litfl.com
- ecgwaves.com
- metealpaslan.com
- medmastery.com
- uptodate.com
- ecgpedia.org
- wikipedia.org
- Strong Medicine
- Understanding Pacemakers